MEFANET Journal 2017; 5(1): 28-39
ORIGINAL ARTICLE
Standardization in medical education: review, collection and selection of standards to address technical and educational aspects in outcome-based medical education
Christos Vaitsis1, Dimitris Spachos2, Matěj Karolyi3, Luke Woodham1,4, Nabil Zary1,5, Panagiotis Bamidis2, Martin Komenda3*
1 Department of Learning, Informatics Management and Ethics, Karolinska Institutet, Stockholm, Sweden
2 Medical School, Aristotle University of Thessaloniki, Thessaloniki, Greece
3 Institute of Biostatistics and Analyses, Faculty of Medicine, Masaryk University, Brno, Czech Republic
4 Institute of Medical and Biomedical Education, St George’s University, London, United Kingdom
5 Lee Kong Chian School of Medicine, Nanyang Technological University, Singapore
* Corresponding author: komenda@iba.muni.cz
Abstract
Article history:
Received 23 May 2017
Revised 22 August 2017
Accepted 15 September 2017
Available online 25 September 2017
Peer review:
Krzysztow Pancerz, Jaroslav Majerník
Download PDF
Background. Modern medical and healthcare curricula represent a highly complex mixture of different disciplines, specialties and pedagogical approaches, the nature of which can be difficult to communicate to key stakeholders. This issue is exacerbated when considering curricula beyond individual institutions at a local, national or international level. To date, there is no standardised way of describing and reporting curricula within Outcome-Based Medical and Healthcare Education.
Methods. We conducted a state-of-the-art review of available technical standards in medical and healthcare education, and identified those most relevant to the field. Based upon this initial pool of standards, we applied a set of selection criteria to identify those standards that were both required and best suited to developing a standardised model for describing medical and healthcare curricula. In concert with this, we conducted a review of common systems in the field to identify the levels of support and compliance with these standards.
Results. We identified standards and specifications from mEducator and MedBiquitous as being most suitable for inclusion in this model. In particular, the MedBiquitous Curriculum Inventory standard, as well as related specifications, are described in detail and proposed for use in best practice implementations.
Conclusions. We propose a standardization approach involving the use of technical standards, compliant systems and standardized vocabularies for the description of medical and healthcare curricula. Such an approach can provide a detailed picture of a curriculum’s structure and address different technical and educational aspects of Outcome-Based Medical and Healthcare Education. The benefits include for faculty, policy and decision makers being able to better evaluate and measure teaching against the required outcomes, institutions to perform structured analyses and being able to compare their curricula, while students can better understand their intended learning.
Keywords
Medical education; healthcare education; outcome-based education; curriculum; standardization; technical standards; standard-compliant systems
Background
In recent years, medical and healthcare higher education institutions are placing more emphasis on creating graduates who are able to deliver high-quality patient-centred care and follow evolving and constantly increasing demands of health care systems. The profile of future health professionals relates closely to a well-structured curriculum that properly combines theoretically focused and clinical-based courses [1,2]. Curriculum designers usually construct their educational programmes in accordance with selected pedagogical approaches suitable for teaching and assessing medical and clinical knowledge and skills. However, balancing courses across the range of medical disciplines (such as Surgical Sciences, Internal Medicine, Diagnostic Sciences, and Theoretical Sciences) represents a significant challenge, due to the variety of medical educational contexts and the multi-faceted character of medical education [3,4].
A unified way of structuring, reporting and expressing the structure of a medical curriculum is required to better understand and communicate that structure to key local, national and international stakeholders. To our knowledge, such a unified way of structuring a medical curriculum is rarely realized or seen at an institutional level within the context of Outcome-Based Medical and Healthcare Education (OBMHE). There is great amount of variation in medical programmes at institutional, national and international levels; different education data formats, levels of detail, description styles, learning outcomes and competencies definitions. This makes it challenging to construct a general, ‘big picture’ overview of OBMHE.
At this level, curricula are supported technically and educationally by individually selected Learning Management Systems (LMS) and thus cover these needs without mechanisms for addressing more than a few perspectives. A different approach, based on data standardization, unification, and common educational content parameterization principles, would allow for the bridging of individual health educational contexts, especially in an era where the mobility of health professionals increases constantly in an international level [5]. With a health professions curriculum as the main tool and by using a common language of understanding progress can be made towards innovations in medical education that promote improved transparency and comprehensibility of educational programmes [6].
The aim of this study is therefore to identify and suggest a standardization approach consisting of a set of technological standards and best practices from standard compliant systems. We anticipate that this approach could be used in an OBMHE context to address: (a) technical needs; as it can be applied in a Curriculum Management System (CurrMS) to allow the educational data to be previewed, extracted and reported in a structured and sophisticated way; and (b) educational needs; as the structured extracted data can be analysed to better understand the educational content and to communicate the reported data for comparison and benchmarking purposes between different OBMHE contexts.
Methods
To accomplish our aim, we reviewed the range of existing standards and specifications in the medical and healthcare education domain. We investigated the standards’ suitability for meeting the above-mentioned needs by constructing a set of criteria to facilitate and support a selection process. Having identified those standards which satisfy the criteria, we described in depth the selected standards by analysing and presenting their structure, functionality, information flow, terminology used, and the requirements for a successful adoption with practical guidelines, along with reflections on their ability to be expanded and implemented in the European outcome-based health education context. Finally, we discuss and address the challenges of transferring and adopting this standardization approach into the European context of health education and the opportunities arising from such an endeavour, thus setting a base for the presented approach to be considered for adoption in outcome-based health educational programmes outside Europe.
Review method
We approached the review and collection phases with the goal of identifying a solution which allows technical standards and medical terminologies to work in concert, and when adopting and applying best practices from standard-compliant systems is suitable for implementation into a CurrMS. Currently used medical terminologies and the challenges of adopting a specific vocabulary that standardizes medical information adequately, were identified in a previous study [7].
To identify the technical standards and standard-compliant systems, we conducted a state-of-the-art review as described by [8]. This method is commonly used to provide an overview of the current knowledge in the field under question and offer new perspectives for future investigation and research. A drawback of this method is that it may distort the overall view of the examined field by only considering developments that took place within a specific time period. We considered that this factor would not materially affect our review because our focus is on a contemporary OBMHE context only, and would therefore only need to consider standards that are in current use or development. Legacy standards, or those that would require repurposing in order to be transferred to a modern health education context would not therefore be suitable for inclusion. Given this, we limited the number of reviewed standards to those specific to health education and constructed a set of selection criteria for both the technical standards and compliant systems. We subsequently chose only those standards which have the ability to work in concert with each other, and which are able to address the technical and educational needs of an OBMHE. Depending on purposes of our study, the attention was paid on up-to-date and reusable solutions, which make access to learning agenda, measurement of improvements and curricula understanding much easier. Based on the selected state-of-the-art review method, we explored those medical and healthcare education standards and specifications published by international professional medical societies, namely the specifications from mEducator Best Practice Network and standards from MedBiquitous Consortium. There are also several other projects active in this particular research area, which unfortunately don’t meet requirements on stable standardised framework (for example: Project Management Curriculum and Resources https://pmiteach.org/teaching-pm/knowledge-module, Scottish Doctor project http://www.scottishdoctor.org), CanMEDS project http://canmeds.royalcollege.ca/en/framework etc.)
Technical standards selection criteria
Our standardization approach attempts to address both technical and educational aspects in medical education. Therefore, the standards must allow the curriculum data to be technically standardized so they can be further reported in a structured format to allow high level analysis for better understanding of the educational content but also to be communicated for comparison and benchmarking purposes. Also, a necessary precondition to this is that the CurrMS where the standards will be integrated must already be used to map [9,10] a health professions curriculum while it incorporates the philosophy of a standards compliant system in an OBMHE context.
Upon initial review of the available data standards relating to healthcare education, we have identified those from mEducator and MedBiquitous as the most appropriate for further examination. Both sets of standards have been developed and used in health education for purposes such as sharing, communication and dissemination of medical curricula [11–13] and are more frequently found to be integrated in LMSs. MedBiquitous standards are widely used in an OBMHE context in medical schools in the United States and Canada. Hence, from the available MedBiquitous standards we will select the ones that are suitable and relevant while we will exclude the standards that are not suitable or appropriate from the final standardization approach based upon specific criteria (Table 1). Criteria C1 to C4 are the ones that can be used to adequately address the needs of structuring, reporting and comparing a curriculum and therefore standards that satisfy one to all of them will be included while standards that satisfy criterion C5 will be excluded as non-appropriate.
Table 1. Criteria for selection of standards
|
Criterion |
Description |
|
C1 |
The standard can be integrated into a CurrMS. |
|
C2 |
The standard can be used to standardize the entire curriculum. |
|
C3 |
The standard can be used to report and communicate the entire curriculum. |
|
C4 |
The standard can be used to standardize a specific part of the curriculum (competencies, learning objectives and outcomes, learning activities and assessment) and is associated and/or works in concert with other standards that satisfy the criteria C1, C2 and C3. |
|
C5 |
The standard is used to report a variety of educational and administrative procedures and processes other than those in criterion C4, does not satisfy the above criteria and/or it is not associated to other standards that satisfy the criteria C1, C2 and C3. |
Standards-compliant system selection criteria
The CurrMSs overview is based on a set of predefined criteria, which help to systematically identify the fundamental standard-compliant system’s characteristics: (i) License type describes the software use and redistribution conditions. We sort systems mainly into two license categories – open-source and commercial; (ii) the ability to support integration of MedBiquitous standards and specifically the ones that satisfy the most criteria in Table 2; (iii) the ability to support integration of the mEducator specification.
Results
Overview of Standards and Systems
Technical Standards: mEducator Best Practice Network
The outputs of the mEducator [14] project are a framework, a software toolbox, guidelines, best practice recommendations and content, which solves the problem of content sharing for medical education. It is based on linked data principles and semantic web technologies. The most important component of mEducator is the standardization schema, namely, the mEducator schema or specification. The mEducator schema makes it possible to discover, retrieve, use, rate, re-use and re-purpose medical educational content irrespective of any LMS usage. Following is a more detailed description of mEducator.
The mEducator project was managed to achieve a number of objectives that focus directly to the development and adoption of the universal description of medical educational content, using modern web technologies: (i) provided tools for medical content publishing, discovery, and retrieval; (ii) analysed policies and mechanisms for content evaluation, rating, renewal, and repurposing; (iii) elaborated on intellectual property rights for digital educational material; (iv) tested the impact of true interoperability, repurposing, enrichment, and embedding of a variety of highly attractive and up-to-date learning resources; provided guidelines and recommendations on how to implement interoperable educational content discovery and retrieval networks; (v) implemented and extended specifications and standards on a critical mass of medical educational content types and provided recommendations for standards adoption and promotion across Europe; and (vi) supported the efficient and seamless sharing and use of formal, specialized, state-of-the-art, and pedagogically sound medical educational content across Europe.
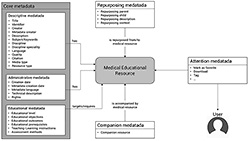
The mEducator target user audience includes three main types of users: (i) medical educators (clinical/non clinical, in academia); (ii) medical students (under- and post-graduates); and (iii) residents and specialized doctors (continuing medical education). One of the main achievements of the mEducator project is the creation of the metadata description scheme and reference model called the mEducator schema. Initially the consortium generated the conceptual model, a process which included an analysis of Healthcare Learning Object Metadata (HLOM) [15], the evaluation of other specifications and standards, a description of the requirements related to repurposed content, along with the respective incorporation of extensions for repurposed content, the refinement of educational aspects and the inclusion of companionship of resources.
During the project, the consortium considered the benefits of Linked Data and the Semantic Web [16], which allow resources to be interoperable with other data sets by reusing and linking to existing knowledge. The mEducator metadata description schema uses ontologies to describe fields, and provides formal naming and definitions for data types, properties, and interrelationships. The full metadata description of each learning object is exposed using the Resource Description Framework (RDF) [17]. RDF was identified as the most appropriate framework to be used for the treatment of the metadata model, since it offers a metadata scheme compliant with the linked data principles. The conceptual model was transformed into an RDF model, which in turn was serialized in eXtensible Markup Language (XML) to be machine-readable. Attention metadata was also considered and the Atom Activity Streams [18] mapping in RDF vocabulary has been extended for full user activity tracking. Using the SPARQL Protocol and RDF Query Language [19] queries can be executed and advanced reasoning performed on the available datasets. Each query can be distributed to multiple SPARQL endpoints (e.g. different web sites that implements the mEducator schema). The complete metadata description schema addresses the requirements and needs for sharing mEducator educational resources. Figure 1 shows the conceptual model.
One of the most important features of the mEducator framework is repurposing. Repurposing refers to the changing of a learning resource initially created for a specific educational context into one that is suitable for a new educational context (or more than one contexts), and should be distinguished from reuse – reuse refers to the use of the same learning resources without any changes. The mEducator consortium has conducted research into various possible types of content repurposing and has established a set of content repurposing contexts and their definitions: (i) repurposing to different languages; (ii) repurposing to different cultures; (iii) repurposing for different pedagogical approaches; (iv) repurposing for different educational levels; (v) repurposing for different disciplines or professions; (vi) repurposing to different content types; (vii) repurposing for different technology; (viii) repurposing for people with different abilities; (ix) repurposing to educational content; and (x) changes in the content itself. The procedure for repurposing medical educational content in general can be complex and may vary greatly from one case to another.
Technical Standards: MedBiquitous Consortium
The MedBiquitous Consortium [20] is an American National Standards Institute [21] (ANSI) accredited developer of information technology standards for healthcare education and quality improvement. MedBiquitous uses XML specifications to create a blueprint of required technology for advancing continuous improvement and lifelong learning for the health professions while maintaining an open process of standards development. The MedBiquitous standards are used to ensure that curricula data concerning competencies, learning and assessment activities, learning objectives and more are structured in a way that can be reported, shared and communicated across health professions education. The standards are focused in all three medical education levels; undergraduate, postgraduate and continuous education of health professionals. We describe below the existing standards with additional information for each of them in the provided references.
Activity Report [22] (AR) provides a standard format for digitally tracking health education and certification activities concerning learning and performance improvement. The standardized data can be used to provide easier and faster document certification, lower administrative time for clinicians and to represent a full picture of health professionals’ accomplishments during the course of their career. Competency Framework [23] (CF) provides a standard format for representing a set of desired competencies. The purpose of the CF standard is twofold; for organizations that publish competency frameworks to do so in a standardized format so it can be integrated into educational systems such as a CurrMS, and for medical and other health professions schools to map their curriculum data to a specific and common set of competencies, enabling a competency-based view of the curriculum and education in general. Curriculum Inventory [24] (CI) provides a data structure that allows one to represent an entire health professions curriculum in a standard format. The purpose of this standard is to promote aggregation and exchange of curriculum data and allows for extensions so that it can be easily communicated. CI uses the CF standard and Competency Object specification (described below) to describe its different components. Healthcare Learning Object Metadata [25] (HCLOM) provides a standard way to describe learning activities and content so as to make it easier to locate, share and integrate learning resources into portfolios and personal health records. Healthcare Professional Profile [26] (HPP) provides a standard format for data concerning the profiles of health professionals. This is useful for accurate updating of credentials data, delivering credentials data to regulatory bodies, institutions and the public and for developing systems to utilise credentials data. MedBiquitous Medical Education Metrics [27] (MEMS) provides a standard format for Continuing Education (CE) outcomes data. The standard is particularly useful for collecting validation data for standardized survey items. A companion specification allows CE providers and outcomes companies to post standardized survey items to a central database. MedBiquitous Virtual Patient [28] (MVP) provides a data structure that describes a Virtual Patient (VP) activity. It is meant to facilitate the creation, implementation and reusing of VPs. Performance Framework [29] (PF) provides a standard format for representing expected levels of performance tied to a specific competency. Competency Object [30] (CO) is a specification that allows discrete competencies, learning outcomes, objectives and other types of educational goals to be represented in a standard format. It is used in concert with the CF standard.
The above listed standards are summarized in Figure 2, in which the MedBiquitous standards architecture is depicted through the associations between the different standards. The associations (connections) are XML Schema Definition (XSD) dependencies/import statements.
Standard compliant systems overview
In the last decade, quality improvement of medical education and training has been emphasised as a concept across higher education institutions due not only to the advent of scientific methods such as data analytics [32], but also due to the need for high quality patient care and elimination of medical errors [20–22]. Various standards, which are usually incorporated into CurrMSs, are created in order to enable quality improvement through tracking of professional achievements, access learning, more effective measures of improvement including the entire curricula comparison, performance and interoperability [6]. To date, standardized frameworks implemented in medicine and other health professions vary in the way they delineate but also in the language used to describe specific learning outcomes and competencies. In this review, we provide an overview of the existing institution-developed as well as commercial CurrMSs, which are specifically focused on medical and healthcare education. Especially, our attention focuses on CurrMSs supporting mEducator specification and MedBiquitous standards.
Ilios [36] is an open-source web-based curriculum management system. It provides features such as managing the curriculum data, sharing materials and outcomes among programs, curriculum mapping and other. Another open-source standard-compliant system is OpenTUSK [37]. It is built on a common web framework called LAMP [38]. Commercial CurrMS 4iQ Solutions platform [39] is interesting because of its Standard integration tool, which allows for the integration of various MedBiquitous standards and the mEducator specification. The Entrada [40] open-source system consists of seven pillars (major functionalities) – curriculum mapping and reporting, academic scheduling, LMS features, assessment and evaluation features, facilitated learner ePortfolio, faculty accountability, community social integration. The MedSIS 3C [41] from Knowledge4you has a set of modules for managing a curriculum and creating reports in a standard-compliant form. It is offered under commercial license. The MedHub system [42], OASIS [43] and one45 [44] allow reporting of data to AAMC using the Curriculum Inventory standard. The last system which is considered in our overview and is also standard-compliant is LCMS+ [45], which provides the possibility of integrating many external systems and tools. The last two CurrMS (OpalQM [46], itsLearning [47]) are not standard-compliant but represent effective tools for managing teaching. We present all the above-mentioned systems and their main differences in Table 3.
Apart from these systems, we have identified more LMSs which mainly support one of the mentioned standards, but provide more or less management of training and educational material services (eMed [48], eMedley [49], E*Value [50], Schoology [51]). These systems have been excluded from consideration because they do not directly support the complex curriculum management effort for delivery and audit of miscellaneous study programmes.
Inclusion/exclusion of technical standards
The selection of standards is described in Table 2. The symbol ‘✔’ indicates satisfaction of a criterion and symbol ‘-’ indicates the criterion has not been met.
Once successfully adopted and implemented, the combination or exclusive usage of the above included standards can support a set of actions to standardize and express a health education’s curriculum. These are: (i) integration into a CurrMS (CI); (ii) use data structures with terminology and vocabulary able to standardize an entire medical curriculum (CI+CF+CO); and (iii) report and communication of standardised curriculum data (CI). CF and CO are referenced from CI and mainly used to standardize a specific part of a curriculum. Therefore, we present here the CI standard.
Table 2. Inclusion/exclusion of standards
|
Standard |
C1 |
C2 |
C3 |
C4 |
C5 |
Decision |
|
Activity Report (AR) |
- |
- |
- |
- |
✔ |
Exclude |
|
Curriculum Inventory (CI) |
✔ |
✔ |
✔ |
- |
- |
Include |
|
Competency Framework (CF) |
✔ |
- |
- |
✔ |
- |
Include |
|
Healthcare LOM (HCLOM) |
- |
- |
- |
✔ |
✔ |
Exclude |
|
Healthcare Professional Profile (HPP) |
- |
- |
- |
✔ |
✔ |
Exclude |
|
Medical Education Metrics (MEM) |
- |
- |
- |
- |
✔ |
Exclude |
|
MedBiquitous Virtual Patient (MVP) |
- |
- |
- |
- |
✔ |
Exclude |
|
Performance Framework (PF) |
- |
- |
- |
- |
✔ |
Exclude |
|
Competency Object (CO) |
✔ |
- |
- |
✔ |
- |
Include |
Curriculum Inventory
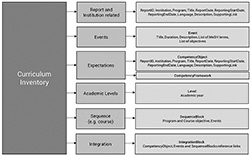
Using the CI standard the curriculum data is reported and represented through an XML file. The XML file is structured through its elements and sub-elements representing the curriculum’s different parts. Other parts of the CI standard are used to specify and make it easier to identify the hosting institution, programme etc. and other to map and express the main curriculum data such as learning activities, learning objectives and courses. All these pieces are put together in CI to provide an overview of how the curriculum is semantically integrated. In Figure 3, follows a diagram of the different entities in the XML CI schema and how they are related to each other to build a CI report. The diagram is adapted from MedBiquitous CI Schema specifications document [52].
A complete example [53] shows CI’s structure along with the referenced CF [54] and CO [55] standards.
Curriculum Inventory: implementation guidelines
For a successful implementation of the CI standard (and its associated standards CO and CF) into a CurrMS that would enable a proper mapping and subsequent communication of the mapped and standardized curriculum, a set of rules must be followed. The rules [56] are distinguished into core (prerequisites) rules that the CO and CF standards must follow and rules that the CI standard itself must follow to be structured accordingly. The CI standard is currently used and mainly implemented by medical and other health professions schools in the US and Canada but the terminology that it provides is mostly universal and can be used to standardize a medical curriculum in different healthcare education settings such as the European or other OBMHE context. However, the standards must be adapted to local settings since the same Events or Expectations can be named differently in different contexts. CI is designed to be flexible and provide the necessary for localisation providing the previously mentioned rules are satisfied. For example, using CI the Expectations are mapped hierarchically. This means that there are Expectations that can be mapped in the lowest level of an Event, Expectations that can be mapped to the next level, the Sequence Block, and Expectations that can be mapped to the entire medical programme. Events and Sequence Block Expectations may be mapped to each other or to Program Expectations or not at all. This information, necessary for the mapping, is pulled from the CurrMS where the CI is to be applied. The map completes when the Expectations from the highest level of the medical programme are mapped to a respective set of competencies, which are provided by the relevant higher education authority under which the medical programme is conducted. For reporting and comparison reasons, CI reports are sent to Association of American Medical Colleges [57] (AAMC). AAMC uses Physician Competency Reference Set [58] (PCRS), which is a unified set of competencies frequently updated. The PCRS competencies are practically used from the CF standard in order to map in the CI the programme level competencies to PCRS and complete the map. Schematically the hierarchy of objectives and competencies mapping in the CI is shown in Figure 4. The Physician Competency Reference Set represents a reference list of common learner expectations in medical and healthcare study programs. Each program contains various sequence blocks, which define an organisational component of the curriculum, such as a course, a module, a learning unit or a learning block (e.g. Anatomy I – Lecture). Finally, each sequence block covers a set of events describing information about educational and assessment sessions that make up the curriculum (e.g. Abdominal Radiology).
Of course, instead of PCRS (and mainly for localization purposes) any other set of competencies provided by the respective higher education authority can be used within the CF standard to map the CI programme level competencies to a higher level as long as it is structured accordingly. Nevertheless, for higher possibilities to maximize the outcomes of implementing the CI standard it is preferable to adapt and match local terminology to the default CI standardized terminology. In this way, the final product, the CI report, can be transferred and communicated more easily outside the borders of one country or continent depending always on the purposes of applying this standardization approach. The full implementation guidelines of the CI standard [59] and the full implementation toolkit containing all the necessary components of CI [60] are accessible on the official MedBiquitous website.
Selected standard compliant systems
Table 3 shows the comparison of selected curriculum management systems in alphabetical order. The majority support at least one of the MedBiquitous standards and specifically the CI standard. On the other hand, fewer systems are compliant with the mEducator specification.
Table 3. Standard compliant systems comparison
|
System name |
License type |
MedBiquitous standard support |
mEducator specification support |
Outcome-based education support |
|
4iQ Solutions platform |
Commercial |
CI |
Metadata description scheme |
Yes |
|
Entrada |
GPLv3 |
CI, CF |
NA |
NA |
|
Ilios |
MIT |
CI, CF |
NA |
Yes |
|
itsLearning |
Commercial |
NA |
NA |
NA |
|
LCMS+ |
Commercial |
CI |
NA |
NA |
|
MedHub system |
Commercial |
CI |
NA |
NA |
|
MedSIS 3CKnowlege4You |
Commercial |
CI |
NA |
NA |
|
OASIS |
Commercial |
CI |
NA |
NA |
|
one45 |
Commercial |
CI |
NA |
NA |
|
OpalQM |
Commercial |
NA |
NA |
NA |
|
OpenTUSK |
ECLv2, GPLv3, LGPLv3 |
CI |
NA |
NA |
NA – not available
Discussion
In this study, we present an approach for standardizing medical and healthcare curriculum data. In an outcome-based education context such as the European OBMHE, the focus is on the final product - the learning outcomes/objectives, competencies - which in turn determines how the medical curriculum’s content is structured and organized in order to adequately address them [61]. We suggest the present standardization approach, which places outcomes/objectives and competencies in the centre, and comprises three unique features to complete the standardization picture: (i) the chosen technical standards; (ii) the best practices from standard compliant systems; and also (iii) the necessary vocabulary for standardizing medical terminology used in medical and healthcare education [7].
Firstly, the selected technical standards (CI, CF and CO) take over the role of providing a way to structure and weave together all related curriculum educational content. That creates a blueprint of activities, objectives and resources, and all its interrelations including: all learning and assessment activities along with teaching and assessment methods; the learning objectives of a single activity (lecture, seminar, written examination etc.); the learning objectives of the parent course where the activity belongs; the parent learning objectives for the entire programme where the courses belong; the parent competencies provided by a higher educational authority for each of the programs; and all learning materials. In this way, the content can be viewed from different perspectives serving different educational needs of involved higher education institutions stakeholders such as decision makers, policy makers, faculty management, teachers, administrators, and students. For example, decision and policy makers as well as faculty management can instantly evaluate if/how the desired higher education board competencies are addressed through the realization of the respective objectives for the entire medical program. Teachers can easily verify whether what they teach is aligned to the curricular objectives and students can see a clear description of their intended learning. Next, a standard compliant CurrMS is required to provide the necessary ground for the standards to be applied. A precondition for a successful standards implementation is that the curriculum data within the CurrMS must be already mapped towards also a standardized medical vocabulary [62]. Thus, having in place a CurrMS that standardizes educational content according to this approach, we can address technical needs by applying high level data analysis to the content using different techniques such as data mining, analytics and visualization techniques [63] for different purposes such as supporting decision making [64] and quality improvement of medical and healthcare education [32].
To the best of our knowledge, within the European OBMHE context, such a standardization effort that addresses these aspects holistically it is not yet in place. The use of this approach has the potential to support research and benchmarking activities, such as systematically and structured analyses and evaluations of health education programmes, and comparisons against other medical curricula that use the same standardization approach. This could support the creation of a unified way of structuring and understanding medical education within the context of European OBMHE or other OBMHE and “shift curriculum mapping and reporting from a somewhat disjointed and institution-specific undertaking to something that is shared among multiple medical schools and across whole medical education systems” [13]. We adopt this approach within the context of the Medical Curriculum Innovations (MEDCIN [65]) project, in which we apply all these concepts in a European OBMHE context in an effort to address these educational and technical aspects. In future studies we will report the challenges and opportunities arising from such an effort setting thus the base for structuring and unifying European OBMHE.
Conclusions
In this paper, we present a comprehensive overview of contemporary technical standards and standard-compliant systems. We recommend an approach in which standards and systems work in concert to address technical and educational needs within the European OBMHE context, applicable to any similar educational context. We select the components of the standardization approach based upon criteria that promote managing, structuring, understanding, reporting and communicating a curriculum and its elements such as learning objectives/outcomes, competencies and learning and assessment methods.
The ultimate outcome of the approach is twofold. At first, it enables medical and general health professions educational programmes to benefit at an individual level by structuring and organizing their curriculum and by being able to systematically describe, model, and store it in standard-compliant structure. Subsequently, it offers the opportunity to communicate the curriculum outside the boundaries of a single institution in a national and international level for sharing, comparison and benchmarking purposes between medical schools and entire health professions educational systems using the same standardization approach. This study is the first in a series of studies that will build and report on the progress of adopting and implementing this approach in the European OBMHE.
List of abbreviations
AAMC: Association of American Medical Colleges
ANSI: American National Standards Institute
AR: Activity Report
CE: Continuing Education
CF: Competency Framework
CI: Curriculum Inventory
CO: Competency Object
CurrMS: Curriculum Management System
HCLOM: Healthcare Learning Object Metadata
HPP: Healthcare Professional Profile
HLOM: Healthcare Learning Object Metadata
LMS: Learning Management Systems
MEDCIN: Medical Curriculum Innovations
MEMS: MedBiquitous Medical Education Metrics
MVP: MedBiquitous Virtual Patient
OBMHE: Outcome-Based Medical and Healthcare Education
PCRS: Physician Competency Reference Set
PF: Performance Framework
RDF: Resource Description Framework
VP: Virtual Patient
XML: eXtensible Markup Language
XSD: XML Schema Definition
Competing interests
The authors declare that they have no competing interests.
Funding
The authors were supported from the following grant project: MEDCIN – Medical Curriculum Innovations (reg. no.: 2015-1-CZ01-KA203-013935), which is funded by the European Commission ERASMUS+ program.
References
1. Fenwick T, Dahlgren MA. Towards socio‐material approaches in simulation‐based education: lessons from complexity theory. Med Educ 2015; 49: 359-367.
2. Dyrbye L, Shanafelt T. A narrative review on burnout experienced by medical students and residents. Med Educ 2016; 50:132-149.
3. Mennin S. Self‐organisation, integration and curriculum in the complex world of medical education. Med Educ 2010; 44: 20-30.
4. Vaitsis C, Nilsson G, Zary N. Visual analytics in healthcare education: exploring novel ways to analyze and represent big data in undergraduate medical education. Peer J 2014; 2:e 683.
5. Wismar M, Maier CB, Glinos IA, Dussault G, Figueras J. Health professional mobility and health systems. Evidence from 17 European countries. European Observatory on Health Systems and Policies; 2011.
6. Komenda M. Towards a Framework for Medical Curriculum Mapping. [Online]. Masaryk University, Faculty of Informatics 2015 [cit. 2016-11-03]. Available at WWW: <http://theses.cz/id/rs7v3c/>.
7. Komenda M, Schwarz D, Švancara J, Vaitsis C, Zary N, Dušek L. Practical use of medical terminology in curriculum mapping. Comput Biol Med 2015; 63: 74-82.
8. Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Inf Libr J 2009; 26: 91-108.
9. Harden R. Curriculum mapping: a tool for transparent and authentic teaching and learning. Association for Medical Education in Europe Dundee; 2001.
10. Komenda M, Víta M, Vaitsis C, Schwarz D, Pokorná A, Zary N, et al. Curriculum Mapping with Academic Analytics in Medical and Healthcare Education. PloS One 2015; 10: e0143748.
11. Smothers V, Greene P, Ellaway R, Detmer DE. Sharing innovation: The case for technology standards in health professions education. Med Teach 2008; 30: 150-154.
12. Mitsopoulou E, Woodham L, Balasubramaniam C, Poulton T, Protopsaltis A, Dietze S. mEducator: multi type content repurposing and sharing in medical education. Acad Subj Cent. Med Dent Vet Med Newsl 2010; 22: 26-28.
13. Ellaway RH, Albright S, Smothers V, Cameron T, Willett T. Curriculum inventory: Modeling, sharing and comparing medical education programs. Med Teach 2014; 36: 208-215.
14. mEducator. [Online]. [cit. 2016-11-03]. Available at WWW: <http://www.meducator.net>.
15. Medbiquitous Healthcare Learning Object Metadata. Specifications and Description Document. [Online]. [cit. 2016-11-03]. Available at WWW: <http://www.medbiq.org/sites/default/files/files/HealthcareLOMSpecifications_pointrelease.pdf>.
16. Mitsopoulou E, Taibi D, Giordano D, Dietze S, Yu HQ, Bamidis P, et al. Connecting medical educational resources to the Linked Data cloud: the mEducator RDF Schema, store and API. 2011.
17. Klyne G, Carroll JJ. Resource description framework (RDF): Concepts and abstract syntax. 2006.
18. Atkins M, Norris W, Messina C, Wilkinson M, Dolin R. Atom Activity Streams 1.0. Abgerufen Am 2011; 22: 2013.
19. SPARQL, Wikipedia. [Online]. [cit. 2016-11-03]. Available at WWW: <https://en.wikipedia.org/wiki/SPARQL>.
20. Medbiquitous. [Online]. [cit. 2016-11-03]. Available at WWW: <http://www.medbiq.org>.
21. American National Standards Institute (ANSI). [Online]. [cit. 2016-11-03]. Available at WWW: <http://www.ansi.org>.
22. Medbiquitous standards: Activity Report. [Online]. [cit. 2016-11-03]. Available at WWW: <http://www.medbiq.org/std_specs/standards/index.html#ActivityReport>.
23. Medbiquitous standards: Competency Framework. [Online]. [cit. 2016-11-03]. Available at WWW: <http://www.medbiq.org/std_specs/standards/index.html#Competencies>.
24. Medbiquitous standards: Curriculum Inventory. [Online]. [cit. 2016-11-03]. Available at WWW: <http://www.medbiq.org/std_specs/standards/index.html#CurriculumInventory>.
25. Medbiquitous standards: Healthcare Learning Object Metadata (Healthcare LOM). [Online]. [cit. 2016-11-03]. Available at WWW: <http://www.medbiq.org/std_specs/standards/index.html#HCLOM>.
26. Medbiquitous standards: Healthcare Professional Profile. [Online]. [cit. 2016-11-03]. Available at WWW: <http://www.medbiq.org/std_specs/standards/index.html#HCProfProfile>.
27. Medbiquitous standards: Medical Education Metrics. [Online]. [cit. 2016-11-03]. Available at WWW: <http://www.medbiq.org/std_specs/standards/index.html#MEMS>.
28. Medbiquitous standards: MedBiquitous Virtual Patient. [Online]. [cit. 2016-11-03]. Available at WWW: <http://www.medbiq.org/std_specs/standards/index.html#MVP>.
29. Medbiquitous standards: Performance Framework. [Online]. [cit. 2016-11-03]. Available at WWW: <http://www.medbiq.org/std_specs/standards/index.html#performance_framework>.
30. Medbiquitous specifications: Competency Object. [Online]. [cit. 2016-11-03]. Available at WWW: <http://www.medbiq.org/std_specs/specifications/index.html#competency_object>.
31. Greene P. Building the Infrastructure for Continuous Improvement: A MedBiquitous Update. [Online] 2016. [cit. 2016-11-03]. Available at WWW: <http://www.docfoc.com/building-the-infrastructure-for-continuous-improvement-a-medbiquitous-update>.
32. Vaitsis C, Hervatis V, Zary N. Introduction to Big Data in Education and Its Contribution to the Quality Improvement Processes. In: Ventura SS (ed). Big Data Real-World Appl. InTech: 2016: 41–64.
33. Wong BM, Levinson W, Shojania KG. Quality improvement in medical education: current state and future directions. Med Educ 2012; 46: 107-119.
34. Wong BM, Kuper A, Hollenberg E, Etchells EE, Levinson W, Shojania KG. Sustaining quality improvement and patient safety training in graduate medical education: lessons from social theory. Acad Med 2013; 88: 1149-1156.
35. Shen B, Dumenco L, Dollase R, George P. The importance of quality improvement education for medical students. Med Educ 2016; 50: 567-568.
36. Ilios: Curriculum Management System. [Online]. [cit. 2016-11-03]. Available at WWW: <https://www.iliosproject.org/>.
37. OpenTUSK. [Online]. [cit. 2016-11-03]. Available at WWW: <http://opentusk.org/about.html>.
38. Open Source Development with LAMP. [Online]. [cit. 2016-11-03]. Available at WWW: <https://www.amazon.com/Open-Source-Development-LAMP-Apache/dp/020177061X>.
39. 4IQ solutions. [Online]. [cit. 2016-11-03]. Available at WWW: <http://www.4iqsolutions.com/>.
40. Entrada. [Online]. [cit. 2016-11-03]. Available at WWW: <http://www.entrada-project.org/>.
41. Knowledge4you. [Online]. [cit. 2016-11-03]. Available at WWW: <http://knowledge4you.com/solutions/medsis3c/>.
42. medhub. [Online]. [cit. 2016-11-03]. Available at WWW: <http://www.medhub.com/>.
43. OASIS scheduling software. [Online]. [cit. 2016-11-03]. Available at WWW: <http://schillingconsulting.com/oasis_scheduling.html>.
44. one45. [Online]. [cit. 2016-11-03]. Available at WWW: <https://www.one45.com/products/>.
45. LCMS. [Online]. [cit. 2016-11-03]. Available at WWW: <https://lcmsplus.com/>.
46. opalQM. [Online]. [cit. 2016-11-03]. Available at WWW: <http://www.opalqm.com/product/>.
47. its learning. [Online]. [cit. 2016-11-03]. Available at WWW: <http://www.itslearning.net/curriculum-management>.
48. eMed. [Online]. [cit. 2016-11-03]. Available at WWW: <https://medprogram.med.unsw.edu.au/emed>.
49. emedley. [Online]. [cit. 2016-11-03]. Available at WWW: <http://www.emedley.com/ecurriculum>.
50. medhub: e*Value. [Online]. [cit. 2016-11-03]. Available at WWW: <http://www.evaluehealthcare.com/solutions/teaching-solutions>.
51. Schoology. [Online]. [cit. 2016-11-03]. Available at WWW: <https://www.schoology.com>.
52. Medbiquitous: Curriculum Inventory Specifications. [Online]. [cit. 2016-11-03]. Available at WWW: <http://www.medbiq.org/sites/default/files/files/CurriculumInventorySpecification.pdf>.
53. Medbiquitous: Curriculum Inventory example. [Online]. [cit. 2016-11-03]. Available at WWW: <http://ns.medbiq.org/curriculuminventory/v1/curriculuminventory.xsd>.
54. Medbiquitous: Competency Framework Specifications. [Online]. [cit. 2016-11-03]. Available at WWW: <http://www.medbiq.org/sites/default/files/files/CompetencyFrameworkSpecification.pdf>.
55. Medbiquitous: Competency Object Specifications. [Online]. [cit. 2016-11-03]. Available at WWW: <http://medbiq.org/sites/default/files/CompetencyObjectSpecification.pdf>.
56. AAMC: Curriculum Inventory. CI Structure & the Competency Framework. [Online]. [cit. 2016-11-03]. Available at WWW: <https://www.aamc.org/download/348854/data/cibusinessrules.pdf>.
57. Association of American Medical Colleges (AAMC). [Online]. [cit. 2016-11-03]. Available at WWW: <https://www.aamc.org>.
58. AAMC: Physician Competency Reference Set (PCRS). [Online]. [cit. 2016-11-03]. Available at WWW: <https://www.aamc.org/initiatives/cir/about/348808/aboutpcrs.html>.
59. Medbiquitous: Curriculum Inventory Implementation Guidelines. [Online]. [cit. 2016-11-03]. Available at WWW: <http://medbiq.org/sites/default/files/files/CI_ImplementationGuidelines.pdf>.
60. Medbiquitous: Curriculum Inventory Implementation Toolkit. [Online]. [cit. 2016-11-03]. Available at WWW: <http://medbiq.org/sites/default/files/files/curriculuminventory_implementation_toolkit.zip>.
61. Harden RM. AMEE Guide No. 14: Outcome-based education: Part 1-An introduction to outcome-based education. Med Teach 1999; 21: 7-14.
62. Komenda M, Schwarz D, Vaitsis C, Zary N, Dušek L. OPTIMED Platform: Curriculum Harmonisation System for Medical and Healthcare Education. Stud Health Technol Inform 2015; 210: 511-515
63. Vaitsis C, Nilsson G, Zary N. Big data in medical informatics: improving education through visual analytics. Stud Health Technol Inform 2014; 205: 1163-1167.
64. Vaitsis C, Nilsson G, Zary N. Visual Analytics in Medical Education: Impacting Analytical Reasoning and Decision Making for Quality Improvement. Stud Health Technol Inform 2015 ;210: 95-99.
65. Medical Curriculum Inovations (MEDCIN) project. [Online]. [cit. 2016-11-03]. Available at WWW: <http://www.medcin-project.eu/>.
Please cite as:
Vaitsis C, Spachos D, Karolyi M, Woodham L, Zary N, Bamidis P, Komenda M. Standardization in medical education: review, collection and selection of standards to address technical and educational aspects in outcome-based medical education. MEFANET Journal 2017; 5(1): 28-39. Available at WWW: http://mj.mefanet.cz/mj-20170523.
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License (http://creativecommons.org/licenses/by-nc-sa/3.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the MEFANET Journal, is properly cited. The complete bibliographic information, a link to the original publication on http://www.mj.mefanet.cz/, as well as this copyright and license information must be included.
![Figure 2. MedBiquitous standards architecture [31] Figure 2. MedBiquitous standards architecture [31]](/res/image/vol5-iss2/20170523-fig02-thumb.jpg)