MEFANET Journal 2017; 5(1): 6-12
ORIGINAL ARTICLE
Virtual patient cases: to use or not to use? Exploring creators' attitudes against their use in the undergraduate medical curriculum
Areti Z. Karasmani*, Panagiotis E. Antoniou, Panagiotis D. Bamidis
Lab of Medical Physics, Medical School, Aristotle University of Thessaloniki, Thessaloniki, Greece
* Corresponding author: aretikarasmani@gmail.com
Abstract
Article history:
Received 22 April 2016
Accepted 9 December 2016
Available online 31 March 2017
Peer review:
Sheetal Kavia, Natalia Stathakarou
Download PDF
Background: The problems and difficulties in students' education that arise from the existing undergraduate curriculum at the medical school of Aristotle University of Thessaloniki (AUTH) urged the academic staff members to the pursuance of new pedagogic approaches that could revitalize medical education practice. The educational programs "mEducator", "ePBLnet" and "Ariadne" that run at AUTH laid the foundations for the development of a plenty of virtual patient (VP) cases. A VP is an innovative computer simulation method that can motivate students to occupy themselves with their studies and perfect their skills. Unfortunately, despite the indisputable advantages of embedding VPs to the lessons, their utilization is neglected during the educational process at AUTH.
Objective: The purpose of this study was to explore the reasons for which VP authors do not use their own VP cases. Why even VP authors avoid VPs' exploitation and in this way they forsake the insistent efforts they made through the rigorous process of VPs' creation?
Methods: After study' s authorization, 35 academic staff members, who had previously developed their own VPs, signed an informed consent and fulfilled a specially designed questionnaire, mainly consisted of closed questions (answer: yes/no) about the possible causes of VPs' dereliction.
Results: Some 77% of participants granted that they do not utilize their own VP cases. Almost 56% of them admitted that the lack of proper infrastructures (computers, projectors) and Internet connection in the lecture rooms impede VPs' use. Specifically, some 33% acknowledged the absence of access to the Internet as the only reason of VPs' abandonment. Almost 52% claimed that they do not have enough time in the courses for covering the great curriculum. Moreover, almost 30% sustained that the great number of students in the lessons enables all of them to conduct a fruitful discussion. Almost 15% asserted that they do not exploit VPs due to the combination of the above two reasons.
Conclusions: Undoubtedly, VPs' embracement can upgrade medical education practice. According to this study, infrastructural in conjunction with organizational problems subvert VPs' utilization during the pedagogic process. The institutions should strive for these problems' resolution in order to facilitate medical education modernization and complete future curriculum transformation.
Keywords
Virtual patient; simulation; medical education; attitudes; undergraduate curriculum
Introduction
Background
The undergraduate curriculum at the medical school of Aristotle University of Thessaloniki (AUTH) has a duration of twelve semesters (six years) and is divided into the preclinical and clinical courses [1].
The medical students follow the preclinical courses in the first three years of their studies. They attend lectures and participate in laboratory exercises about basic sciences, such as Biology, Genetics, Biochemistry, Medical Physics, Physiology, Anatomy, Histology, Pathology, Microbiology and Pharmacology [1].
Unfortunately, the enormous number of lectures in contrary with the few laboratory exercises have as a consequence that there is no clear correlation between the basic science lessons and their value for the daily medical practice. As a result, students are often unable to use their basic sciences' knowledge in their clinical training [2].
In the following three years, they take the clinical courses, which include Internal Medicine, General Surgery, Urology, Orthopedics, Pediatrics, Psychiatry, Gynecology, Anesthesiology and other medical specialties. In these courses, they attend lectures and they commence having contact with patients, as they are taught about taking a medical history, performing a physical examination, ordering biochemical and radiological exams and making a differential diagnosis [1,2].
The foremost difficulty that all the trainees are called to confront in this period of their studies is the fact that they have to practice their skills for first time on real patients, where there is a very real possibility of harming the patients due to complete lack of clinical experience. Additionally, too many students are responsible for the care of one single patient, because of the great number of them trained at every university hospital. In this way, after their graduation, the new doctors indicate that they do not feel confident about their skills, since they did not practice some of them even once or they did not repeat them enough times in order to hammer them in. During their courses it is, also, highly unlikely to face a variety of medical diseases of all the medical specialties, that are not common or belong to the category of the rare diseases and learn how to recognize and encounter all of them efficiently, especially when their patient's life is jeopardized.
Furthermore, the immense curriculum that has to be studied during both the preclinical and the clinical courses make it impossible for students to remember the significant information that is essential to comprehend and exploit so that they will be effective as students and as doctors later [2].
All the problems and difficulties underlined above created the urgent necessity to attempt to upgrade the providing medical education with the purpose of equipping the students with a diversity of skills. The use of simulation of different clinical scenarios is the most modern alternative pedagogic method which is scientifically proven and acceptable (through many clinical trials and studies) that it increases students' interest in medicine in very important grade and it assists them to assimilate medical knowledge and enhance and finally perfect their skills [3-21].
Nowadays, many types of simulation are utilized during the educational process. For instance, there are simulators, manikins or automatic robots, which simulate human functions such as breathing or responding to stimuli, that are exploited in many medical universities worldwide in order to facilitate students' education [16,19,22].
Another kind of medical simulation is a virtual patient (VP). The definition of a VP was provided by Medbiquitous, which is an international organization, established by John Hopkins Medicine, which aims to the creation of open technological standards for medical education and in which AUTH participates as a member [23]. According to this organization, "a VP is defined as an interactive computer simulation of real-life clinical scenarios for the purpose of medical training, education, or assessment" [24].
Prior work
In Greece, the first VP cases were developed by several medical teachers and their research associates at the Medical School of AUTH under the educational projects "mEducator", "ePBLnet" and "Ariadne", which intended to contribute to the curriculum transformation by embracing the utilization of new technologies during medical students' education [2].
"mEducator – Multi-type Content Repurposing and Sharing in Medical Education project" was sponsored by the eContentplus 2008 programme and carried out by fourteen European partners between 2009 and 2012. The target of this project was to gather educational material and create interlinked data, which can be effortlessly shared and exploited [25].
Many European and Asian medical schools collaborated for "ePBLnet EU project" to promote the use of VP cases, give prominence to the significance of Problem Based Learning and set up a network of Medical Education Centers in Georgia, Ukraine and Kazakhstan [26].
The program "Ariadne" was implemented inside the medical school of AUTH and the participants were academic staff members who were trained in developing VPs. The program's goal was to introduce the new technologies in the medical education and highlight the VP cases as a new teaching approach [27]. An example VP screen from this project is demonstrated in Figure 1.
In general, numerous academic staff members of the medical school of AUTH (professors, assistant professors, lecturers and associate researchers) developed plenty of VP cases, which concern clinical scenarios of Internal Medicine, Pediatrics, Gynecology, Neurology, Oncology, Biopathology, Otorhinolaryngology, Radiology, Urology, Ophthalmology, Dermatology, Cardiology, Forensics, General Surgery, Vascular Surgery, Plastic Surgery and Pediatric Surgery. All the medical students of AUTH have free access to the VPs via Internet and they can practice to them at any time they wish [27].
There is no doubt that the creation of a VP is a thorny process, which requires much time and effort from the authors. All the VP cases were developed in agreement with Medbiquitous VP standards. The Medbiquitous VP standard includes five fundamental components [24]:
- the "VP data", which are information of the medical history and the medical examination related to the scenario and are necessary for the users to complete the VP case successfully,
- the "media resources", which are digital files, such as X-rays, respiratory sounds and are also correlated to the scenario,
- the "data availability model", which specifies how the data are exposed,
- the "activity model", which determines the way that the users are able to interact with the VPs and
- the "VP player", which exposes the VP to the user [2,24].
For the development of the VPs, firstly, the authors had to create the medical scenario. Subsequently, they designed the labyrinth of the scenario by converting educational material to digital form with the assistance of Visual Understanding Environment (VUE). VUE is a software program that was made available by Tufts University [2,24,28]. At the end of the procedure, the authors used the program OpenLabyrinth as a VP player. OpenLabyrinth is a free web application for creating and deploying interactive web based scenarios like VPs [2,24].
Objective
Unfortunately, although the authors had really time-consuming and complicated courses for developing VPs and despite the dedicating and great effort they made, VPs are not extensively used during medical students' practice at AUTH. Hence, the aim of this article is to scrutinize the reasons that even VP authors do not exploit the fruits of their own efforts, the VP cases that they created through laborious work. Why VPs consist such a neglected education approach in the Medical School of AUTH, while they are widely utilized globally and they can ameliorate and modernize medical education practice?
Methods
After the study's authorization by the Ethics Committee of AUTH, an email was sent to all the VP authors in order to inform them about the conducting survey. Afterwards, the VP creators received another email that contained as attachments an informative brochure, which described minutely the characteristics of the survey, a consent form which had to be signed by all the authors, who would decide to participate in our survey and a specially designed questionnaire about the reasons they might do not utilize their own VP cases.
The form consisted of seventeen questions. The first two questions concerned the participants' experience on computer use and informatics before the VPs' development. Specifically, one question inquired on how familiar the participants were with the use of technology such as Internet, computers and e-learning techniques. The participants had to assess themselves by grading their knowledge with one (no familiarity with new technologies) to five (absolute familiarity). The other question was whether they knew what VPs were. In addition, the participants had to grade their acquaintance with technology after the VPs' creation with one to five and record whether they applied their VPs to their lessons.
Figure 1. How does a VP screen look like?
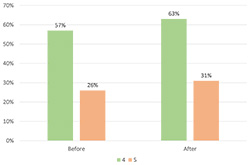
Figure 2. Percentage of participants grading their knowledge of new technologies with four and five before and after VPs' development
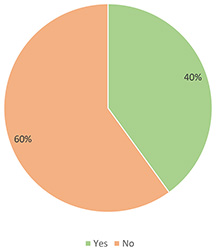
Figure 3. Did you know what Virtual Patients were before their development?
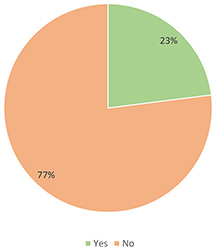
Figure 4. Do VP authors exploit their own VP cases?
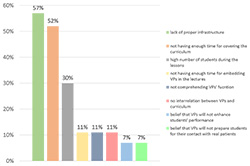
Figure 5. Reasons for not using VPs
In case the authors responded negatively to this question, they were required to reply to a series of closed questions (they had to answer yes or no) which attempted to explore the probable explanations of disregarding VPs' exploitation. They were asked if they do not use VPs due to lack of time for preparing their presentations and embedding VPs in their lectures or lack of time for covering the curriculum during the lessons. Moreover, they were inquired if difficulties in comprehending VPs' way of function, deficiency in proper infrastructure (access to the Internet, computer, projector) or dearth of interrelation between the VPs and the curriculum of every course discourage them from utilizing VP cases. The other questions concerned if the reason they do not take advantage of the VPs is that they believe that the great number of students during the classes does not allow conduction of discussion for the VPs or that the students will face obstacles with VPs' use or they will not pay the requisite attention to this alternative educational method. Furthermore, they were asked if they avoid VPs' utilization because they consider that VP cases are not going to stimulate students' interest in their lessons, improve their performance or prepare them effectively for their contact with real patients. Finally, they were required to answer if there are other reasons except the above that could justify that VP cases remain unexploited. If the authors responded positively, then they had to clarify these reasons. Table 1 summarizes the entirety of the questionnaire that was presented to the participants.
Table 1. Questionnaire
|
Questions that concern authors' experience before VPs' development |
Answers |
|
How familiar with technology (Internet, computers, |
no familiarization: 1-2-3-4-5: complete familiarization |
|
Did you know what VPs were? Answer: |
Yes/No |
|
Questions about authors' experience after VPs' creation |
Answers |
|
How familiar with technology (Internet, |
no familiarization: 1-2-3-4-5: complete familiarization |
|
Do you exploit VP cases during your lessons? |
Yes/No |
|
If you answered "no" to the previous question: |
... |
|
You do not have enough time for preparing |
Yes/No |
|
You have difficulty comprehending their way of function? |
Yes/No |
|
The courses have short duration and you do not |
Yes/No |
|
They do not relate to the curriculum of every lesson? |
Yes/No |
|
You do not have the proper infrastructure (computer, |
Yes/No |
|
You believe that the great number of students during the of discussion and reaching decisions about the clinical scenarios? |
Yes/No |
|
You think that the students will struggle with VPs' use? |
Yes/No |
|
You suppose that they will not stimulate |
Yes/No |
|
You believe that the students will not pay the necessary |
Yes/No |
|
You consider that they will not enhance students' performances? |
Yes/No |
|
You think that they will not prepare efficiently |
Yes/No |
|
For other reasons? |
Yes/No |
|
If you answered "yes", what are these reasons? |
... |
Results
Thirty-five academic staff members responded to our call and they fulfilled our questionnaire. The answers to the questionnaires were statistically analyzed and evaluated. Figures 2 and 3 reveal that some 57% and almost 26% of participants graded their knowledge of new technologies with four and five respectively before the VPs' development, while 40% of them admit that they did not know what VPs were. Almost 63% and some 31% of them graded their familiarity with technology with four and five respectively after completion of the courses they had for VPs' creation.
As Figure 4 demonstrates, some 77% of participants recorded that they do not exploit their own VP cases during their lessons. Almost 56% of them responded positively to the question if they do not utilize VPs because of deficiency in infrastructure, such as proper computers and projectors and Internet connection in the classrooms and amphitheatres. Particularly, some 33% alleged that the lack of access to the Internet during the lessons is the only cause of neglecting VP cases. Almost 52% of them contended that the great curriculum they have to cover during the short courses demoralize them from using VPs. Moreover, almost 30% asserted that the great number of students in the classrooms does not allow the involvement of all of them in the conduction of impactful discussion about the decisions that have to be made about the clinical scenarios. Specifically, almost 15% maintained that they avoid VPs' use due to the combination of the above two reasons. Some 11% claimed that they do not have enough time for integrating the VP cases into their lectures, while also some 11% struggle with comprehending VPs' function or do not utilize them as VP cases do not conform to the educational program of every lesson. Some 7% believe that VPs are not salutary and they are not going to enhance students' performance or prepare them successfully for their clinical training, while there were no positive answers to the question if they think that VPs are not going to trigger students' interest in Medicine. Furthermore, no one answered positively to the questions if they believe that the students will encounter difficulties with VPs' use or they will not give proper regard to this educational method. A summary of these results is visualized in Figure 5.
Conclusions
Undoubtedly, VP cases are able to revitalize medical education practice as they indubitably spark students' interest in the scientific field of Medicine and conduce to widening their knowledge and optimizing their skills [3-21]. Nevertheless, it has to be emphasized that VPs and generally medical simulation methods do not supersede real patients, but they broaden medical experience that is gained through daily care of patients [29,30].
Despite the indisputable benefits of VPs and the development of a plenty of them at AUTH, their use has not been established yet during the educational process at the Medical School of AUTH. This study designates infrastructural and organizational problems as the most consequential reasons that VP authors do not avail themselves of their own clinical scenarios. Appropriate computers and projectors as well as access to the Internet are unavailable in the classrooms and the amphitheatres of the Medical School. In addition, students are divided into large groups to have their courses and there is an unquestionable disproportion between the courses' duration and the enormous curriculum.
It is of crucial importance that institutions aspire to the solution of these problems promptly. The lecture rooms have to be equipped with modern infrastructure and the educational program should be flexible in order to contribute to the perfection of students' skills.
Policy formers have to attend painstakingly to these infrastructural and organizational problems and surmount these obstacles immediately in order VPs' use to be encouraged at the medical school of AUTH. The adoption of VPs' exploitation as a vital pedagogic method will be conducive to emending and revolutionizing medical education practice and will definitely urge to a radical curriculum transformation that will harmonize with the global educational standards.
Acknowledgements
We would like to warmly thank all the VP authors who participated in our survey and filled in our questionnaire with the intention of redounding to medical education's revolutionization at the Medical School of AUTH.
Conflicts of Interest
There is no conflict of interest.
References
1. Study guide of School of Medicine of Aristotle University of Thessaloniki. [Online]. Available at WWW: <http://qa.auth.gr/en/studyquide/200000057/current>.
2. Dafli E, Bamidis PD, Dombros N. Pilot virtual patient application in Greek medical education. Archives of Hellenic Medicine 2010; 27(5): 803–810.
3. Tachecí I, Ryška A. Virtual cases in internal medicine education. Mefanet J 2015; 3(1): 21–27.
4. Cook DA, Erwin PJ, Triola MM. Computerized Virtual Patients in Health Professions Education: A Systematic Review and Meta-Analysis. Acad Med 2010; 85:1589–1602.
5. Consorti F, Mancuso R, Nocioni M, Piccolo A. Efficacy of virtual patients in medical education: A meta-analysis of randomized studies. Comput Educ 2012; 59(3): 1001–1008.
6. Kleinert R, Plum P, Heiermann N, Wahba R, Chang D-H, Hölscher AH, Stippel DL. Embedding a Virtual Patient Simulator in an Interactive Surgical lecture. J Surg Educ 2016; 73(3): 433–441.
7. McCarthy D, O’Gorman C, Gormley GJ. Developing virtual patients for medical microbiology education. Trends Microbiol 2013; 21(12): 613–615.
8. Cook DA, Triola MM. Virtual patients: a critical literature review and proposed next steps. Med Educ 2009; 43: 303–311.
9. Sobocan M, Klemenc-Ketis Z. Family Medicine Education with Virtual Patients: a Qualitative Study. Acta Inform Med 2015; 23(4): 202–205.
10. Kleinert R, Heiermann N, Wahba R, Chang D-H, Hölscher AH, Stippel DL. Design, Realization, and First Validation of an Immersive Web-Based Virtual Patient Simulator for Training Clinical Decisions in Surgery. J Surg Educ 2015; 72(6): 1131–1138.
11. Okuda Y, Bryson EO, DeMaria S Jr, Jacobson L, Quinones J, Shen B, Levine AI. The Utility of Simulation in Medical Education: What Is the Evidence? Mt Sinai J Med. 2009; 76: 330–343.
12. McCarthy D, O’Gorman C, Gormley G. Intersecting Virtual Patients and Microbiology: Fostering a culture of learning. Ulster Med J 2015; 84(3):173–178.
13. Bateman J, Allen M, Samani D, Kidd J, Davies D. Virtual patient design: exploring what works and why. A grounded theory study. Med Educ 2013; 47: 595–606.
14. Lehmann R, Bosse HM, Simon A, Nikendei C, Huwendiek S. An innovative blended learning approach using virtual patients as preparation for skills laboratory training: perceptions of students and tutors. BMC Med Educ 2013; 13: 23.
15. Leung JYC, Critchley LAH, Yung ALK, Kumta SM. Evidence of virtual patients as a facilitative learning tool on an anesthesia course. Adv Health Sci Educ 2015; 20: 885–901.
16. Lopreiato JO, Sawyer T. Simulation-Based Medical Education in Pediatrics. Acad Pediatr 2015; 15: 134–142.
17. Jäger F, Riemer M, Abendroth M, Sehner S, Harendza S. Virtual patients: the influence of case design and teamwork on students’ perception and knowledge – a pilot study. BMC Med Educ. 2014; 14: 137.
18. Cendan J, Lok B. The use of virtual patients in medical school curricula. Adv Physiol Educ 2012; 36(1): 48–53.
19. Kleinert R, Heiermann N, Plum PS, Wahba R, Chang D-H, Maus M, Chon S-H, Hoelscher AH, Stippel DL. Web-based immersive virtual patient simulators: Positive effect on clinical reasoning in medical education. J Med Internet Res 2015; 17(11): e263.
20. Nicolaidou I, Antoniades A, Constantinou R, Marangos C, Kyriacou E, Bamidis P, Dafli E, Pattichis CS. A virtual emergency telemedicine serious game in medical training: A quantitative, professional feedback-informed evaluation study. J Med Internet Res 2015; 17(6): e150.
21. Pantziaras I, Fors U, Ekblad S. Training with virtual patients in transcultural psychiatry. Do the learners actually learn? J Med Internet Res 2015; 17(2): e46.
22. Allen A. Tripler army medical center hosts simulation center open house. [Online]. Available at WWW: < http://www.army.mil/article/127148/>.
23. MedBiquitous's mission and scope. [Online]. Available at WWW: <http://www.medbiq.org/about_us/mission/index.html>.
24. Smothers V, Azan B, Ellaway R. ANSI /MEDBIQ VP.10.1-2010 MedBiquitous Virtual Patient Specifications and Description Document. 2010.
25. Objectives of mEducator. [Online]. Available at WWW: <http://www.meducator.net/?q=content/objectives>.
26. Brief description of ePBLnet project. [Online]. Available at WWW: <http://www.epblnet.eu/content/brief-description>.
27. Program Ariadne. [Online]. Available at WWW: <http://vp.med.auth.gr/ariadne>.
28. Visual Understanding Environment. [Online]. Available at WWW: <http://vue.tufts.edu/>.
29. Proaño A, Ruiz EF. What medical students need: Virtual patients or real patients? 2015; Med Teach, 37:2, 202-202.
30. Poulton T, Balasubramaniam C. Virtual patients: A year of change. Med Teach 2011; 33(11):933–937.
Please cite as:
Karasmani AZ, Antoniou PE, Bamidis PD. Virtual patient cases: to use or not to use? Exploring creators' attitudes against their use in the undergraduate medical curriculum. MEFANET Journal 2017; 5(1): 6-12. Available at WWW: http://mj.mefanet.cz/mj-20160422.
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License (http://creativecommons.org/licenses/by-nc-sa/3.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the MEFANET Journal, is properly cited. The complete bibliographic information, a link to the original publication on http://www.mj.mefanet.cz/, as well as this copyright and license information must be included.