MEFANET Journal 2017; 5(1): 13-18
ORIGINAL ARTICLE
New educational program “Medicine + PBL” – requirement of time or innovation?!
Nana Shavlakadze1*, Nino Tabagari2, Gulnara Shelia1, Nato Alavidze1, Irine Phkhakadze1
1 Medical Faculty of Akaki Tsereteli State University, Kutaisi, Georgia
2 David Tvildiani Medical University, Tbilisi, Georgia
* Corresponding author: nanashavlakadze@hotmail.com
Abstract
Article history:
Submitted 8 February 2016
Revised 17 July 2017
Accepted 27 July 2017
Available online 9 August 2017
Peer review:
Sheetal Kavia, Panagiotis Antoniou
Download PDF
Changes that are made in education during last decade is the guarantee of Georgia’s integration in the European educational space. Accordingly, medical education must be based on the international standards and must be result oriented to get the competitive graduates on the medical market.
Within the new medical educational program “Medicine + PBL” a new Problem Based Learning (PBL) teaching method has been implemented on the faculty of Medicine at Akaki Tsereteli State University (ATSU) during 3 years. The innovations are the basic medical and clinical disciplines that are integrated in the program, also their supporting courses and social disciplines. The structure of the program is conditionally divided into three steps: teaching basic, preclinical and clinical subjects and clinical teaching and clinical practicing stages.
Medical Doctor (MD) program is a “hybrid” program, where so called PBL cases are integrated into medical disciplines. In order to reach the learning outcomes, which includes the development of knowledge, practical skills/habits and values, the program is based on “4 spiral” model: the progress of knowledge and awareness, the doctor-patient communication, "public and population health" and "personal and professional growth". PBL teaching method and format strengthens the quality of program integration and provides the Medical Doctor with possibilities of effective achievement of Learning Outcomes (LOs).
Keywords
PBL; case study; integration
Introduction
New methodologies of medical education are very rapidly developing in the modern world alongside with other fields of science. Modern medicine is inconceivable without the latest technologies, which require adequate knowledge. The process of obtaining and creating the knowledge begins in the medical classes. It is the place, where two main systems: theory and practice should be merged. This is difficult, but not impossible. Various innovative methods are implemented broadly in order to facilitate the processes of Medical Education. The teaching strategies and curricula of high medical schools are based on the recommendations and guide lines worked out by International Association for Medical European Education (AMEE) [1].
In Medicine it is important to develop not only basic theoretical and clinical science knowledge but also to obtain clinical skills, and to establish ethical values and attitudes very important for the profession [2]. Within the Bologna Process frame, competencies of basic medical education is determined according to the learning outcomes, which are developed according to the TUNING/MEDINE demands.
Nowadays, the result-oriented education is considered optimal in terms of the country’s requirements, as it is based on the international standards of medical education, which in fact provides successful and competitive certified doctors.
Faculty of Medicine of Akaki Tsereteli State University was founded 20 years ago. It trains students in three fields: Medical Doctor (one-step high medical educational program), Doctor in Dental Medicine (one-step high medical educational program) and Pharmacist (with the degree of Bachelor / Master).
There are Georgian and English language Medical educational programs. It is one-step program with the duration of 6 years, comprising 360 credits, and equals the second level of the higher education.
The Faculty has a long-term history of cooperation with European partners. This gave us an opportunity to have high qualified teaching staff, which have been trained in the top rated universities of the world, to have in the latest modern electronic classes, to have research laboratories equipped with the newest facilities, all these make it possible to conduct electronic, distance learning with the partner universities.
To provide the quality assurance of medical education we permanently conduct the survey of our employers, graduates and students. For this purpose, last survey was done with total number of 130 from the second (49), fourth (40) and fifth (41) year students. They were asked just two simple questions: Do you like the learning process and what would you change in the educational process?
The results showed that in general, students are content with the educational process and despite positive attitudes, 47% of interviewed complained about the educational process resentment and stated that they would like the following improvements: to get more information from a lecturer (41%), more visual materials (48%) and to discuss more clinical cases (93%). The last request which implies desire and importance to do more case-study learning was underlined by the vast majority of the students (93%).
It should also be mentioned that during the last decades Georgia has been in the atmosphere of permanent changes, and then it becomes easy to guess that something was not done as it was necessary and some additional changes or improvements were required?!
The goal
The quality of basic medical education, as the most important preliminary condition for a successful medical practice, and its relevance with international standards is a major problem of the health system to ensure optimal operation of Georgian healthcare system. The adoption of this in cooperation with foreign counterparts appeared to be more easily achievable.
In cooperation with our foreign colleagues (St George's University of London, Aristotle University of Thessaloniki and University of Nicosia) and with the help of Tempus grant project 530519-TEMPUS-1-2012-1-UK-TEMPUS-JPCR “Establishment of the Supra-Regional Network of the National Centres in Medical Education, focused on PBL and Virtual Patient (ePBLnet)” Georgian Universities (David Tvildiani Medical University and Akaki Tsereteli State University, Faculty of Medicine); Ukraine (Sumy State University and Zaporozhye State Medical University); Kazakhstan (Astana Medical University and Karaganda State Medical University) started the modernization of the basic stages of the existing educational programs. The changes were based on the introduction of a new learning method - problem-based learning [3].
Although the problem-based learning, or PBL counts more than 2 decades of its existence and it is the most approved and recommended training method not only on medical but other faculties of the world’s leading universities, it is still “innovative” and strange for the post-soviet countries [4–8].
The way to achieve the goal
The ePBLnet group, created on the Faculty of Medicine of ATSU in accordance to the requirements of the Tempus project started working in five different directions: modernization of the curriculum, translation and adaptation of dozens of cases, training of tutors, setting up the online library and creating PBL training infrastructure. What is more, all these had to be done in a short period of time in about 1.5 year. The implemented changes were mainly focused on the teaching / learning methods, in particular, the problem-based learning, as a relevant methodology of a new “study week”. The “PBL Group” of Akaki Tsereteli State University designed quite a new integrated curriculum in the process of modernization of the old one, which, in its turn, caused development of a new training strategy based on a new study approaches, aims, environment, new systems for assessment and evaluation. As a result a new one-step high medical educational program "Medicine + PBL" was created.
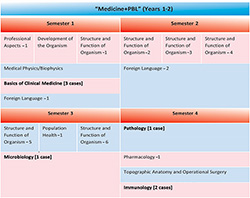
Figure 1. Number of PBL weeks in new MD Program and distribution of cases by semesters
Figure 2. Basic stage (semester I–IV) in the new MD Program
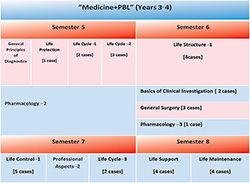
Figure 3. Preclinical and clinical stage (semester V–VIII) in the new MD Program
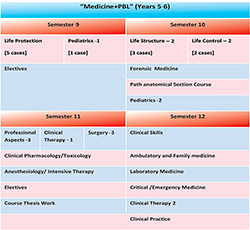
Figure 4. Clinical internships stage (semester IX–XII) in the new MD Program
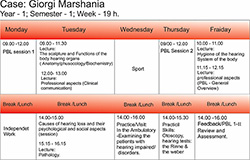
Figure 5.The PBL week of a patient (G.M.) with hearing impairment
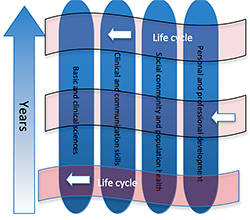
Figure 6. Vertical integration – a spiral curriculum
Results
A new high medical educational program of ATSU is personalized and competence-based, characterized by vertical integration (of 6 years long) on basic training, pre- and clinical stages. The teaching and learning process of the program is designed in the way, which brings the students to their future medical activities as close as possible.
The basic concept of the educational program implies a student’s deep understanding of a profession. At any stage of training, ranging from basic to clinical sciences, a student analysis obtained information / knowledge in terms of clinical practices. All these became possible through distributing PBL weeks (49 PBL weeks) from I to X semesters.
New program structure
The program integrates basic medical and clinical sciences as well as their supporting courses (e.g. biophysics), social sciences (e.g. history of medicine, professional aspects, etc.); which is necessary for a modern doctor to receive general professional education / promotion. Thus the program ensures reaching scientific competencies and obtaining clinical skills for the MD students.
Teaching courses are maintained unchanged for II, XI, XII semesters, while the rest of the courses mostly were grouped into 6 main modules: Life Cycle, Life Protection, Life Support, Life Maintenance, Life Structure, Life Control and are adjusted in accordance to issues considered by cases.
Some cases were distributed among various Basic and Clinical courses. Accordingly, new program systematized and integrated them (PBL cases) in accordance to the above mentioned modules, as well as embedding in same Basic (e.g. Microbiology/Immunology) and Clinical Courses.
Particularly, organization structure of the program is conventionally divided into the following stages:
Stage I (semester I–IV) Basic: It focuses on the structure and function of a human’s main systems (Anatomy, Histology, Biochemistry, Physiology), which are mostly presented in a modular organization and based on a horizontal integration of the Basic Medical Sciences around the systems (Structure and Function of Organism 1,2,3,4,5,6) (Figure 2). At this stage human development is taught (Human Genetics, Embryology, Cytology) and the most important professional aspects for future physicians are introduced based on the Case (PBL Weeks). At this stage of the study, a student studies the issues focused on the population health which is organized in the special module (Epidemiology, Hygiene, Medical Statistics, Medical Physiology and Sociology), as well as the disease-causing mechanisms and its development (Pathology, Microbiology and Immunology). The name of this phase The stage of basic medical sciences is only conventional. It contains a significant part of clinical medicine and population health, which is also supported by PBL training. The basic part of the program and 7 PBL weeks embedded in it, on the one hand, is a good base for teaching the program in PBL format in the future stages. In addition, more issues of clinical “practice” can be discussed and realized. This stage also includes the introductory materials essential for studying the basic and clinical sciences of the human organism systems (human development, the structure and function of an organism, Pathology, Topographic Anatomy and Operative Surgery, Immunology), which, in turn, is the basis for the utilization of the fundamental medical subjects.
Stage II (semester V–X) pre- and clinical stage study, which is mostly organized on understanding of important aspects of Human Health and morbidity as are: Life cycle (Sexual aspects of health and morbidity; Sexual development and health; Regulation of fertility; Preconception and Prenatal Care), Life Structure (Rheumatology and Orthopedic medicine), Life Control (Neurology, Psychiatry, Nutrition), Life Support (Cardiology, Pulmonology, Ophthalmology,Otorhinolaryngology) and maintenance (Gastroenterology, Nephrology, Urology, Endocrinology), Life Protection (Infectious diseases with parasitology, Virusology, Hematology, Oncology, Clinical immunology-allergology). This phase of teaching is carried out by organizing a number of relevant disciplines in general training modules and respective PBL sessions are participating (compulsory) in the training format. This stage of study also contains non-modular teachings in the disciplines (General Principles of Diagnostics, Pharmacology, General Surgery, Basics of Clinical Investigation, Pediatrics). The most important part of this stage of learning is to organize the contents of the module with involving clinical cases and PBL study week, which enables the integration of knowledge in essential basic sciences determined by the case and the contents of its (the case) clinical “part” (anamnesis, symptoms, researches, interpretation, management, communication with a patient and population health issues, etc.) in such a way that the knowledge obtained at the basic stage of learning contributes to “revise”, “understand in the context” and more in-depth study (concepts of basic and clinical sciences and their interrelationship). An important aspect of this stage is also a gradual development of the issues included in the module (“Life Cycle 1, 2” in the 5th semester, “Life Cycle 3” in the 7th semester) which means to move gradually from the linear cases to more difficult branched cases (where the “price” of the decision is very high and in case of wrong choices, the group of “students-doctors” harms the patient). It significantly develops the student's decision-making skills.
Stage III – (semester XI–XII) clinical clerkship for clinical practice, which is mostly a stage of general specialization for clinical practice (for the relevant positions of the certified doctors: an assistant of a doctor, passing exams in residency, etc.), when the students train their clinical skills mostly on a clinical base.
“PBL Week” model/credit/assessment
One credit involves 25 hours of which 15–17 hours are intended for contact and 8–10 hours – for students’ independent work.
PBL week is structured as follows 3 PBL tutorials (Monday and Thursday mornings, Friday afternoon – summarizing) + teaching sessions (Tuesday, Wednesday and Friday mornings) + clinical attachment and/or a visit to the skills lab (Tuesday or Wednesday afternoon) + practical sessions; assessment at the end of PBL week and periodically experts forum (note: considering a particular case specificity the structure is slightly adjusted).
The assessment of a student in MD program is multicomponental (activity, attendance, daily testing, essay, presentations, PBL, surveys, final exam).The evaluation of the learning in the PBL format is also a part of the ongoing assesment and includes: the assessment of the PBL training level, logical thinking / reasoning, communication (with colleagues / patients) and clinical skills. It (above mentioned) has 10% share in the final evaluation of the student.
Discussion
ATSU’s MD program frame realizes the so-called “Hybrid” Program (integration of the medical disciplines and knowledge into modules with PBL participation /implementation, and without them: certain parts of the program are non-modular); it is important to describe “the way” of reaching the results of the program that describes the “own” spiral in terms of the development of the student's knowledge, skills and values :
The whole program can be presented as one spiral in terms of the knowledge and understanding progress, which is practically continuous from the stage I till the end of the learning process. It involves learning valuable issues of basic medical and clinical sciences and understanding them according to the context: Introduction – a horizontally integrated module (stage I, e.g.: The Structure and Function of an Organism-4 “Cardiovascular”) + followed by modules organized on the bases of important issues of human norms and pathology (stage II – pre- and clinical study stage, e.g.: “Life Support – Cardiology”),which ends with a practice in a general specialization (stage III).
II spiral represents a very important part of a future doctor’s professional competences, which can be described under the name of the patient-doctor communication, which implies the understanding and training very important aspects (which covers all structure and organization of the program through focusing on PBL, e.g. Professional Aspects 1, followed learning in PBL format, clinical studies and practice.)
III spiral conventionally represents “Social, Community and Population Health”. It also begins with a teaching in theoretical and PBL format (Population Heath – 1), develops in context (contexts – specialization and/or child/adult/elderly, epidemiology, etc. These issues are discussed almost in every PBL cases. See PBL week) and creates the possibility to develop the learning outcomes of a certified doctor gradually (in this part).
IV spiral “Personal and professional development” is also developing step-by-step (it is supported by theoretical courses, e.g. Professional Aspects 1) and also promotes the possibility to reach the very important goal of the educational program of a certified doctor – „Doctor as a professional” (MEDINE 2).
So, PBL method and format enhances the degree of the program integration, provides possibilities for effective achievement of learning outcomes of MD program, particularly through spiral organization of the program content.
At last, we can say, that learning progress is an outcome of multiple factors, some directly related to formal courses and some to informal and self-directed learning.
And we can be sure in ATSU a new medical program “Medicine + PBL” is benefit for students: this program increases integration level and complexity, it requires more self-directed learning in unstructured environment; PBL educational format increases their responsibility, reflection, teamwork skills and personal knowledge including increased understanding the “value” of an error and motivates them on life-long learning.
Note: The new medical program “Medicine + PBL” was successfully accredited in 2015 and the enrolment of students officially started in 2016.
Acknowledgements
These changes were supported by the Tempus 530519-TEMPUS-1-2012-1-UK-TEMPUS-JPCR project. The authors would like to thank all participants of the project, and especially to Professor Terry Poulton and members of his team.
References
1. AMEE Guide 60-97.
2. Spencer J1, Blackmore D, Heard S, McCrorie P, McHaffie D, Scherpbier A, Gupta TS, Singh K, Southgate L. Patient-oriented learning: a review of the role of the patient in the education of medical students. Medical Educ 2000; 34(10): 851-857.
3. Establishment of the Supra-Regional Network of the National Centers in Medical Education, focused on PBL and Virtual Patients. Available at WWW: <http://www.epblnet.eu/>.
4. Barrows HS. Problem-based learning in medicine and beyond: A brief overview. New Dir Teach Learn 1996; 68: 3-12.
5. Farley J, Erickson JD, Daly HE. Ecological Economics: a Workbook for Problem-Learning. Island Press: Washington DC 2005.
6. Neville AJ. Problem-based learning and medical education forty years on. A review of its effects on knowledge and clinical performance. Med Princ Pract 2009; 18(1): 1-9.
7. Problem-Based Learning Curriculum A Success For Medical School [online]. Medicalnewstoday.com. [cit. 2012-11-16]. Available at WWW: <http://www.medicalnewstoday.com/releases/55419.php>
8. Severiens SE, Schmidt HG. Academic and social integration and study progress in problem-based learning. High Educ 2008; 58: 59–69.
Please cite as:
Shavlakadze N, Tabagari N, Shelia G, Alavidze N, Phkhakadze I. New educational program “Medicine + PBL” – requirement of time or innovation?! MEFANET Journal 2017; 5(1): 13-18. Available at WWW: http://mj.mefanet.cz/mj-20160208.
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License (http://creativecommons.org/licenses/by-nc-sa/3.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the MEFANET Journal, is properly cited. The complete bibliographic information, a link to the original publication on http://www.mj.mefanet.cz/, as well as this copyright and license information must be included.