MEFANET Journal 2016; 4(1): 26-32
ORIGINAL ARTICLE
A new online software tool for pressure ulcer monitoring as an educational instrument for unified nursing assessment in clinical settings
Andrea Pokorná1,*, Jiří Jarkovský2, Jan Mužík2, Soňa Vasmanská1, Simona Saibertová1, Petra Krejčiříková1
1 Department of Nursing, Faculty of Medicine, Masaryk University, Brno, Czech Republic
2 Institute of Biostatistics and Analyses, Faculty of Medicine, Masaryk University, Brno, Czech Republic
* Corresponding author: apokorna@med.muni.cz
Abstract
Article history:
Received 11 March 2016
Accepted 30 March 2016
Available online 5 April 2016
Peer review:
Jaroslav Majerník, Dagmar Tučková
Download PDF
Data collection and evaluation of that data is crucial for effective quality management and naturally also for prevention and treatment of pressure ulcers. Data collected in a uniform manner by nurses in clinical practice could be used for further analyses. Data about pressure ulcers are collected to differing degrees of quality based on the local policy of the given health care facility and in relation to the nurse’s actual level of knowledge concerning pressure ulcer identification and use of objective scales (i.e. categorization of pressure ulcers). Therefore, we have developed software suitable for data collection which includes some educational tools to promote unified reporting of data by nurses. A description of this software and some educational and learning components of the tool is presented herein. The planned process of clinical application of the newly developed software is also briefly mentioned. The discussion is focused on the usability of the online reporting tool and possible further development of the tool.
Keywords
Pressure ulcers; monitoring; uniform assessment; nursing education; data collection; incidence
Introduction
The possibility of analysing the occurrence of pressure ulcers (PU) in patients is an important issue, but in neither the Czech Republic nor internationally is there any uniform methodology for collecting the necessary data that would sufficiently help monitor patients with PU. Most of the PU assessment methods are based on the local know-how of the individual departments or managers and healthcare providers, or they are performed within isolated local prospective and retrospective studies. In most studies the evidence-based classification of PU prepared by the Pressure Ulcer Advisory Panel (EPUAP) is not followed. Thus, sharing of data and comparison of incidence or prevalence data nationwide and even internationally is impossible. In clinical settings without any systematic, ongoing and validated pressure ulcer (PU) registration system, estimating the incidence and prevalence of pressure ulcers will mostly prove an academic and time-consuming exercise, one leading to imprecise estimations [1]. Nonetheless, information on PU occurrence is considered an indicator of healthcare quality and is important for assessing the costs of providing healthcare connected to the occurrence of PU and their consequences (prolonged hospitalization, increased costs of treatment, influence on the patient’s quality of life etc.) [2–4]. In the Czech Republic, there is no database specifically designated for providing unambiguous data on the prevalence and incidence of PU. Furthermore, until now there has not been any uniform platform for data collection concerning PU at the national level. The aim of the presented project (“The register of decubitus ulcers – integration strategy for monitoring and preventive interventions on the national level”) is to establish a standardized methodology and define it uniformly for PU reporting, as well as to prepare a useful electronic tool for monitoring of PU which is to be piloted in three university hospitals in the Czech Republic. The authors are aware that the real incidence of pressure ulcers is underestimated in the administrative data (i.e. in the local registry of adverse events or incident reporting or in the National Registry of Hospitalized Patients – NRHOSP). So, these project activities aim to stress the importance of collecting PU prevalence and incidence data as an effective measure of healthcare and patient outcomes and to identify facility trends for quality and safety evaluation. As project leaders understand that prevalence rates are commonly cited to suggest the development of relevant and innovative care, pressure ulcer incident data is likely to be a better indicator of an organization’s performance in pressure ulcer prevention and damage minimization [1]. Hospital-acquired pressure ulcers (HAPUs) remain a serious iatrogenic problem threatening patient safety and there is need to recognize whether the wound was formatted before admission to the hospital or during the hospitalization. The relationship between patients and direct care staff who have an impact on HAPUs is, however, imprecise, conceptually problematic and operationally difficult [5]. The data must be collected in a uniform manner to capture the scale of wound care. The conventional approach is to record details of ulcer care such as treatment strategies, dressings, antibiotics, analgesics, investigations, hospital admissions and surgical interventions at each patient contact over the period from the first presentation to wound healing [6].
All important details could be monitored, stored for a long time and also retrieved easily only through a well-planned electronic monitoring system which is user-friendly, allows extraction of important data concerning delivery of care and will not increase the burden on healthcare givers (especially nurses). Another aspect which must be taken into account is the lack of training for a unified assessment of PU (not all hospitals in the Czech Republic use the suggested evidence-based EPUAP classification). Another factor is the insufficient use of objectifying scales for assessing the overall condition of the patient by nurses in the clinical setting.
Methods
The article presents a newly prepared electronic software tool (database) for monitoring PU incidence in the clinical setting. The possible benefits and risk of the collected data and uniform evaluation of the patients with PU is discussed. Particularly the elements and components enabling education of nurses concerning the uniform evaluation of PU and patients’ overall status are highlighted. The presented software electronic tool is intended to be useful for objective recording of patient characteristics and uniform PU classification. This tool should not increase the workload and burden on nurses, but rather to enable nurses to gain further experience and expertise, as well as to monitor the influence of preventive clinical processes of care on HAPU incidence and prevalence.
General description of data collection system
Data on PU will be stored in a database system which was originally based on a modified version of the TrialDB system [7–9]. This online system has undergone changes in layout and structure, which has made data entry even more convenient, while security measures have been maintained at the same level as in previous versions. Data security within the registry is of key importance, and special attention has been paid to this issue.
The system has been designed as a robust basis for collection of a large amount of data in clinical trials and/or clinical registries, and it is fully customizable to the structure of the project. The online application is accessible to users via their web browsers. The security of individual records within the registry is guaranteed via anonymized data collection. Each patient’s identity is replaced with a number (ID) which does not allow any backward identification of that person. The unequivocal identification of the patient is known only to the attending physician or to an authorized health care professional.
The main advantages of this system involve centralized administration, uniform appearance of forms for data collection in all registries and easy development of new, extending functions. The basic characteristics of the system are:
- The system is very user-friendly: all data are entered via web forms which are analogous to paper collection (classical CRF). Thus, nurses could use it even as a bedside evaluation.
- The data can be entered into the registry from any computer connected to the internet and equipped with a standard web browser (it must support encrypted communication over a 128-bit SSL protocol).
- No additional software needs to be installed on the client’s computer.
- Only authorized persons have access to the registry, using their login and password.
Data in the registry are de-identified, i.e. the patients’ records are kept under codes (ID) which exclude any chance that the person might be identified. In this way, the system meets all valid rules on the protection of personal data.
All data transfer is encrypted in order to prevent any potential abuse during the transfer. Data can be exported for authorized users as a local database for further processing. Users can print the filled forms or save them in a local computer in MS Excel format.
The system of user rights is one of key functions in the administration of user accounts. Apart from this, automatic logout is done after a predefined period of user inactivity (i.e. when the nurse has to leave the nursing room and go to the patient’s room or to another patient). This function is aimed to prevent misuse of an unoccupied computer if the user forgets to log out.
An encryption protocol is used for data transfer between the user and the central database to prevent tapping of the communication between the client and server (for example, interception of the user login and password). For this reason, any communication between the client and server is realized via the secure protocol HTTPS, using SSL (Secure Socket Layer) encryption.
In order to provide maximum data security, other security measures have been taken by the provider (Institute of Biostatistics and Analyses – IBA), involving mainly the security of the provider’s network and the server itself. These measures include firewalls (separating both database and application servers from the internet), regular monitoring of the system, monitoring changes in configuration, physical protection of the server room, etc.
Additional measures have been taken to prevent potential data loss or damage in the case of unexpected events, which are not directly related to information technology. These measures involve a fire-stop system, air-conditioned server rooms, etc.
Both system configuration and the data stored within it are subject to regular backup. Therefore, even in the case of a system breakdown, the entire system including the data can be promptly restored.
Description of some specific components enabling nurse education in the PU data collection system
As mentioned above, the software tool contains some components and applications to help nurses use appropriate evaluation processes and improve the accuracy of monitoring of patients with PU. The information about the patients is divided into two main sections. The first section covers information about the overall status of the patients (using objective tests, i.e. the Activity of Daily Living Test, Glasgow Coma Scale, and Body Mass Index which are commonly used in the majority of Czech healthcare facilities). This part is identified as anamnesis of the patients and it is the first part of patient registration. Data collected there could be used from the common internal hospital record of the patient in cases where this tool is implemented in the internal hospital electronic system (IHEC). The following variables are recorded: date of birth, gender, age, healthcare department where the patient is hospitalized, date when the information was recorded (date of evaluation of the patient), code of diagnosis according to the ICD-10, mobility and self-sufficiency, ability to collaborate, psychological status, height and weight for the possibility of evaluating nutritional status (Body Mass Index – BMI). The system can also record any possible long-term complication of patient status which could be compounding factors for formation of HAPU. What is of great importance is that all information which has to be reported is selectable (as tick boxes or multiple-choice items) and nurses do not have to remember any scales or classifications (i.e. for BMI, nurses could report information about height and weight and BMI is automatically calculated, or they could directly choose the BMI according to verified data from patient documentation).
Figure 1. Automatic calculation of Norton scores according to specified data
Figure 2. Manually entered data – entering account details (helping table)
Figure 3. Classification of PU (helping figures)
Figure 4. Differential classification of PU and IAD (helping table)
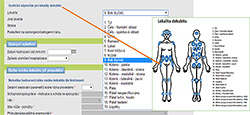
Figure 5. Localization of pressure ulcers (helping picture)
The second part of registration is focused directly on description of the pressure ulcer. The following variables are recorded concerning PU:
- Identification data (workplace where PU was detected and, if different, workplace where PU was formatted).
- Important dates and the time sequence (initial date of hospitalization and number of days from the beginning of hospitalization until detection of an individual pressure ulcer during the hospital stay).
- Connection or linkage with the performance of an operation (surgery).
- Risk evaluation (Norton score) at the beginning of the care and before discharge or transfer (or death) of the patient.
- Preventive strategies (before and after the identification of PU).
- Treatment strategies (immediately after the identification of PU and finally a summary of treatment strategies at the end of care).
- Detailed information about PU which should be reported during the entrance examination when the PU is identified and for the final examination at the end of care (description: size of PU, category, local complication and periwound skin, localization of PU – only for the initial assessment).
In what follows we will present only the components which are the most useful for nurse education and learning.
Risk assessment
The PU risk assessment tool is a system for recording factors about the patient that would increase their risk of developing a PU. These factors are then scored. It is essential that risk assessment be conducted as early (ideally within 8 hours after admission) and as accurately as possible. Assessment of the risk of PU is done on the basis of the Norton scale as this is the most commonly used scale Czech healthcare facilities. Even with the standard use of the Norton scale, there is no single scoring system used in all Czech hospitals and therefore the learning tool for nurses was implemented in the developed online collecting system. Nurses can directly specify data about patient status (i.e. age, mobility, incontinence, or psychological status) and the Norton scale score is automatically calculated. In situations when nurses cannot identify all the data, but they have verified data from previous patient records, they can directly report the Norton score (see Figure 1). In both above mentioned cases, they can make use of help in the form of readable tables (see Figure 2).
Classification of pressure ulcers
The precise and accurate classification of PU is essential for selection of appropriate preventive and therapeutic strategies. However, there is still a lack of consistency in the evaluation of stage/category of PU in clinical settings. Therefore, a further and very important tool for nurses, which corresponds to the newest evidence-based recommendations of EPUAP, has been prepared (see Figure 3). In connection with the identification of the stage/category of PU, also differential diagnostics of incontinence associated dermatitis (IAD) or other lesions (i.e. friction lesion of skin tears) are problematic. The helping and learning tool for differential diagnostics is presented in Figure 4.
Localization of pressure ulcers
Although it may be considered that the location of a PU and its correct identification is underestimated and downplayed in relation to care planning, it is an essential part of effective evaluation and quality management as well as making the appropriate choice of preventive and therapeutic strategies. The last educational tool that we would like to present should help nurses to record the right area and localization of PU (see Figure 5). The most frequent confusion in the location of the PU was identified from retrospectively analyzed patient records in the gluteal region and sacrum. So, nurses could use a picture with a numerical designation of the location and simply record it accurately.
Ethical considerations
The purpose and procedure of this project, voluntary participation, guaranteed anonymity, and the possibility of withdrawing at any time were explained to the subjects (nurses and nursing managers involved in development of the software tool). Ethical permission for the project activities from the hospitals involved was obtained.
Discussion
Nurses, midwives and other non-medical health workers form the bulk of the clinical health workforce and play a central role in all health service delivery systems. There is a potential to improve healthcare quality if nurses and other healthcare staff routinely use the best available evidence in their clinical practice. Since many of the factors perceived by health workers as barriers to the implementation of evidence-based practice (EBP) are found at the organizational level, it is crucial to devise and assess the effectiveness of organizational infrastructures designed to promote EBP among nurses [10]. One very good tool for improvement of the organizational structure and for supporting EBP is simplification of the recording of patient data in a unified fashion. The use of objectifying tests and scales in a uniform manner should help ensure a better understanding and transfer of information in a multidisciplinary team. A number of nurses working today in clinical practice have studied the issue of PU in an “old-fashioned” manner and they do not know exactly how to obtain new information or how to implement the knowledge obtained in lifelong learning. We must also emphasize that the process of knowledge translation is slow, i.e. the translation of research findings into practice [11,12], and it is common problem also in the case of pressure ulcers. Because of this, there is a pressing need for simplified learning strategies that will not serve as barriers for nurses and could increase their knowledge in a non-threatening form for an objective assessment of patients. Pressure ulcers are considered avoidable incidents, but sometimes they occur even if the care is perfect and nurses need to have the evidence in the form of simple and quick records concerning the care rendered. All PU should be investigated to identify the circumstances surrounding PU development using root cause analysis techniques (RCA). This approach seeks to understand the underlying causes and could bring a comprehensive view (i.e. environmental context) of how the incident happened. Therefore, an exact record of data is essential. The authors of the newly developed online reporting system for PU are aware that healthcare professionals have used differing grading systems to describe the severity of PU in the Czech Republic. A global guideline has been developed by the European Pressure Ulcer Panel (EPUAP), National Pressure Ulcer Panel (NPUAP) and Pan Pacific Pressure Injury Alliance (PPIA) [13] and these guidelines are implemented in the online reporting tool presented here. Accurate evaluation of PU is important because the cost of care increases with the severity of PU as the time of healing is longer and the incidence of complication is higher in more severe cases [14,15]. As we know that wound assessment should be comprehensive, systematic and evidence-based, we have followed the recommended framework “Triangle for Wound Assessment” which aims to simplify the evaluation process for all healthcare workers [16]. A systematic approach in assessment and reporting data should help to overcome the barriers to healing as proven by national registries in Sweden [17] and help promote continuity of care. The nature of nursing tasks and interventions has led to a high demand for software that supports long-term bulk data collection, storage and evaluation, as this is a way to save time which is needed for patient care, especially when lack of staff is a big challenge. The benefits of reporting systems have been summarized also by recent work, where special attention has been paid to the five key challenges that explain why incident reporting has not reached its potential: poor processing of incident reports (triaging, analysis, recommendations), inadequate engagement of professionals (especially physicians), insufficient subsequent visible action, inadequate funding and institutional support of incident-reporting systems and inadequate usage of evolving health information technology [18]. Therefore, from the authors’ point of view the human resources (nurses and other healthcare workers’ opinions) and their behaviour and attitudes are important components for the functioning and effectiveness of the online reporting system. Another systematic review has proven that still little is known about the effectiveness of the incident-reporting systems. Some evidence of single-loop learning has been found and there was insubstantial evidence for enabling double-loop learning, that is, a cultural change or a change in mindset [19]. Thus, the authors of this new online reporting tool are aware that it is important to know about the view of users concerning electronic reporting systems. We cannot predict that the system will have a positive effect by changing staff attitudes and knowledge. Nevertheless, the way in which the system is introduced and the training to support its introduction could contribute to a cultural change. Another aspect that must be taken into account is the computer literacy of nursing staff. Some nurses are reluctant users of Information and Communications Technologies (ICT). This factor needs to be managed sensitively, because the experience of the benefits of using ICT and electronic patient records influence their acceptability [20,21] and the implementation processes. For the above mentioned reasons, the long-term implementation plan (at least 6 months) was carefully prepared to implement online monitoring tools. This period will include seminars and workshops, as well as feedback mechanisms (an anonymous questionnaire survey and interviews) to evaluate the satisfaction of target users with the implemented online monitoring tool. There is always one scheduled group seminar for the entire clinic planned, during which the system and methodology of collecting and reporting data will be presented. Two workshops will be subsequently organised for each unit and department where the participants will try assessment of pressure ulcers and their record under the scientific supervision of an expert guarantor from each hospital (project team member). We need to know the nurses’ views on the system in terms of usability (the system cannot be too slow or too fast, reporting cannot be time-consuming, etc.). For the future development of this tool on the local level in each hospital, it is desirable to evaluate the influence of computerization on staff mobility (as this is a commonly-presented problem [22]) and the possibility of sharing data among the various hospital and inpatient settings that are involved. As this tool has been prepared as an educational one, we expect that the finally evaluated dataset will be implemented in the internal electronic hospital reporting system and there is also the possibility of modifying it for tablet users.
Strength and limitation
Data protection and authentication are crucial in clinical software and collection of patient data in a healthcare setting. For this electronic software tool (prepared primarily as an educational tool), nurses are required to use a username and password. The authors of the developed software tool expect that for the clinical implementation, it would be more suitable to implement collection of data into the internal hospital informational/electronic system (IHEC) to ensure better accessibility of data and also for the possibility of using data which already exists about individual patients according to Czech legislation. This should decrease the burden on nurses and allow them to spend more time with patients as the final version of collection tool (dataset) will be implemented as a part of the real information system used in each hospital.
Conclusion
We have developed a software tool which will be primarily used for testing and validation in three university hospitals in the Czech Republic (Military University Hospital Prague, University Hospital in Pilsen and General University Hospital in Prague). At least one project team member is working (mostly at the managerial level) in all of the above-mentioned hospitals and is organizing or leading the education of nurses in usage of the electronic tool and in using objective scales or scoring tests to monitor overall patient status and also the local status of pressure ulcers (face to face workshops and seminars, feedback activities). Notwithstanding, the electronic tool on its own supports self-learning and includes several features to help nurses in situations where it is difficult to decide how to report collected data or classify the patient or pressure ulcer.
Acknowledgement
The authors would like to thank the nurses who participated in creation of the new electronic tool and final dataset for pressure ulcer monitoring (constructive criticism of the dataset components). They appreciate the active approach of these nurses and their willingness to cooperate in development of the new monitoring tool.
This work was supported by the Ministry of Health of the Czech Republic under grant no. 15‑29111A “The register of decubitus ulcers – integration strategy for monitoring and preventive interventions on the national level”. All rights reserved.
Conflict of interest
The authors state that there is no conflict of interest.
References
1. Collier M. Pressure ulcer incidence: the development and benefits of 10 year’s-experience with an electronic monitoring tool (PUNT) in a UK Hospital Trust. EWMA J 2015; 15(2): 15-20.
2. Gunningberg L, Hommel A, Bååth C, Idvall E. The first national PU prevalence survey in county council and municipality settings in Sweden. J Eval Clin Pract 2013; 19(5): 862-867.
3. Demarré L, Van Lancker A, Van Hecke A, Verhaeghe S, Grypdonck M, Lemey J, Annemans L, Beeckman D. The cost of prevention and treatment of pressure ulcers: A systematic review. Int J Nurs Stud 2015; 52(11): 1754-1774.
4. Demarré L, Verhaeghe S, Annemans L, Van Hecke A, Grypdonck M, Beeckman D. The cost of pressure ulcer prevention and treatment in hospitals and nursing homes in Flanders: A cost-of-illness study. Int J Nurs Stud 2015; 52(7): 1166-79.
5. Clarke S, Donaldson NE. Nurse staffing and patient care quality and safety. In: Hughes RG (ed). Patient Safety & Quality: An Evidence-Based Handbook for Nurses. Agency for Health Care Research & Quality, Rockville 2008: 1-25.
6. Harding K, Posnett J, Vowden K. A new methodology for costing wound care. Int Wound J 2013; 10(6): 623-629.
7. Nadkarni PM, Brandt C, Frawley S, Sayward FG, Einbinder R, Zelterman D, Schacter L, Miller PL. Managing attribute--value clinical trials data using the ACT/DB client-server database system. J Am Med Inform Assoc 1998; 5(2): 139-151.
8. Nadkarni PM, Brandt CM, Marenco L. WebEAV: automatic metadata-driven generation of web interfaces to entity-attribute-value databases. J Am Med Inform Assoc 2000; 7(4): 343-356.
9. Nadkarni PM, Marenco L. Easing the transition between attribute-value databases and conventional databases for scientific data. Proc AMIA Symp 2001; 483-487.
10. Flodgren G, Rojas-Reyes MX, Cole N, Foxcroft DR. Effectiveness of organisational infrastructures to promote evidence-based nursing practice. Cochrane Database Syst Rev 2012; 15(2): CD002212.
11. Balas EA, Boren SA. Managing clinical knowledge for healthcare improvements. In: Bemmel J, McCray AT (eds). Yearbook of Medical Informatics 2000: Patient-Centered Systems. Schattauer Verlagsgesellschaft: Stuttgart 2000: 65-70.
12. Rogers E. Diffusion of Innovations. 5th Edition. Simon and Schuster: New York 2003. ISBN 978-0-7432-5823-4.
13. National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers: Quick Reference Guide. Cambridge Media: Osborne Park 2014. ISBN-10: 0-9579343-6-X.
14. Dowsett C, Groemann NM, Harding K. Taking wound assessment beyond the edge. J Wound Care 2012; 21(6): 261-266.
15. Delay C, Chambers T, Beldon P, Benbow M, Fletcher J, Fumarola S, Guy H, Nixon H, Price J, Purser K, Stubbs N, Way L, Weafer K, members of TVS Pressure Ulcers Working Group. Achieving consensus in pressure ulcer reporting. J Tissue Viability 2012; 21(3): 72-83.
16. Dowsett C, Protz K, Drouard M, Harding KG. Triangle of Wound Assessment. Made easy. [On-line] Wounds International, 2015. Available at WWW: <http://www.woundsinternational.com>
17. Öien RF, Ragnarson Tennvall G. Accurate diagnosis and effective treatment of leg ulcer reduce prevalence, care time and costs. J Wound Care 2006; 15(6): 259-262.
18. Mitchell I, Schuster A, Smith K, Pronovost P, Wu A. Patient safety incident reporting: A qualitative study of thoughts and perceptions of experts 15 years after 'To Err is Human' BMJ Qual Saf 2016; 25(2): 92-99.
19. Stavropoulou C, Doherty C, Tosey P. How effective are incident-reporting systems for improving patient safety? A systematic literature review. Milbank Q 2015; 93(4): 826-866.
20. De Veer AJE, Franke AL. Attitudes of nursing staff towards electronic patient records: a questionnaire survey. Int J Nurs Stud 2010; 47(7): 846-854.
21. Stevenson JE, Nilsson GC, Peterson GI, Johansson PE. Nurses experience of using electronic patient records in everyday practice in acute/inpatient ward settings: a literature review. Health Informatics J 2010; 16(1): 63-72.
22. Li J, Westbrook J, Callen, J. Georgiou, A. The role of ICT in supporting the disruptive innovation: a multisite qualitative study of nurse practitioners in emergency departments. BMC Med Inform Decis Mak 2012; 12: 27.
Please cite as:
Pokorná A, Jarkovský J, Mužík J, Vasmanská S, Saibertová S, Krejčiříková P. A new online software tool for pressure ulcer monitoring as an educational instrument for unified nursing assessment in clinical settings. MEFANET Journal 2016; 4(1): 26-32. Available at WWW: http://mj.mefanet.cz/mj-20160311.
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License (http://creativecommons.org/licenses/by-nc-sa/3.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the MEFANET Journal, is properly cited. The complete bibliographic information, a link to the original publication on http://www.mj.mefanet.cz/, as well as this copyright and license information must be included.